A common antibiotic used to treat liver disease could give rise to an “almost untreatable” superbug, scientists warned in a new study.
The antibiotic, rifaximin, has enabled the global emergence of vancomycin-resistant enterococcus faecium, or VRE, a superbug that frequently causes serious infections in hospitalised patients, according to an eight-year-long study published in the journal Nature.
The international team of researchers behind the study warn that the use of rifaximin is driving bacterial resistance to daptomycin, one of the last effective treatment options against VRE infections.
The findings challenge the long-held belief that rifaximin poses “low risk” for causing antibiotic resistance.
The researchers emphasise the need to better understand the negative impacts of antibiotic use and to reinforce their responsible use in clinical practice.
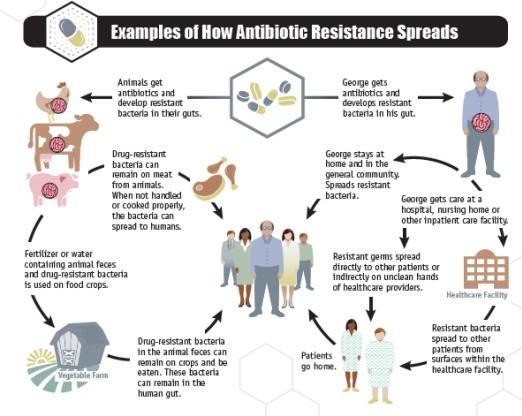
They are concerned that these superbugs could be transmitted to other patients in the hospital.
In the latest study, the researchers found changes in the DNA of daptomycin-resistant VRE that were absent in susceptible strains.
Subsequent analysis revealed that rifaximin’s use caused these changes and sparked the emergence of daptomycin-resistant VRE.
Rifaximin triggers specific changes in an enzyme called RNA Polymerase. The changes lead to a cascade of further alterations in the bacterium’s cell membrane, causing cross-resistance to daptomycin.
“When bacteria become resistant to an antibiotic, it’s a bit like gaining a new ability in a video game, like super-speed. But when exposed to rifaximin, the VRE bacteria don’t just get one boost – they gain multiple abilities, like super-speed and super-strength, allowing them to easily defeat even the final boss,” study co-author Adrianna Turner explained.
“Rifaximin doesn’t just make bacteria resistant to one antibiotic; it can make them resistant to others, including critical last-resort antibiotics like daptomycin.”
The study highlights the benefits of using genomics-based surveillance to detect emerging drug resistance in bacteria.
It says doctors must exercise caution when treating VRE infections in patients who have been taking rifaximin and drug regulatory bodies must consider similar consequences when approving antibiotics.
“Rifaximin is still a very effective medication when used appropriately and patients with advanced liver disease who are currently taking it should continue to do so,” Jason Kwong, another author of the study, said.
“But we need to understand the implications going forward both when treating individual patients and from a public health perspective.”







