
Attention deficit hyperactivity disorder (ADHD) is one of the most common mental health disorders in children, affecting 7.2% of people under the age of 18 worldwide. Many of these children will still have ADHD in adolescence and adulthood.
ADHD is diagnosed using criteria from a document called DSM-5, which include symptoms of inattention, hyperactivity and impulsivity. But it is becoming increasingly clear to researchers that the condition also comes with self-control problems, affecting the ability to regulate emotions.
For example, 2.1% of children with a diagnosis of ADHD also have a mood disorder, such as depression, while 27.4% have an anxiety disorder. Many also have outbursts of verbal or physical aggression.
These previously understudied aspects of the condition are now providing fresh insights into what’s going on in the brain of someone with ADHD – raising hopes for new and improved treatments.
If ADHD is not treated effectively, it can have major effects on a child’s mental health and wellbeing, as well as educational attainment. It may also impact on parents and siblings, as well as other children in the classroom.
So what is the neural link between ADHD and emotions? In our new study, published in Nature Medicine with colleagues at Fudan University in China, we identified a general brain basis – that we call the Neuropsychopathological Factor (NP Factor) – underlying symptoms of multiple mental health disorders, from depression to ADHD.
By using a combination of neuroimaging, cognitive and genetic data, we discovered that many mental health conditions may be linked to a unified, genetically determined problem of “synaptic pruning”.
This process typically occurs in childhood and removes extra synapses (brain structures that help brain cells transmit electrical or chemical signals) in order to ensure that our brains are efficient and connections between regions are optimal.
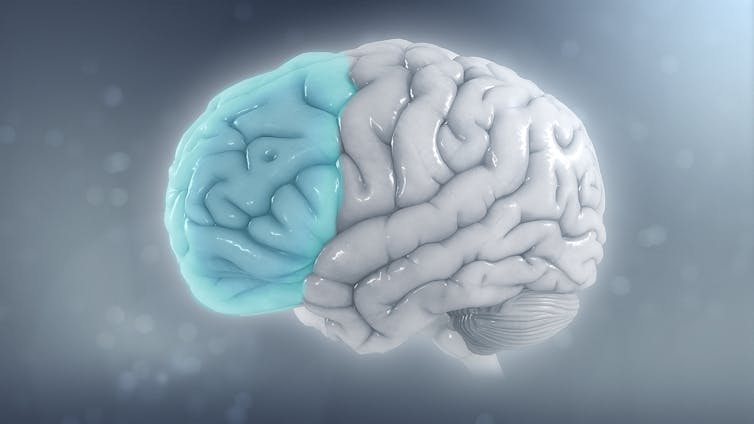
This problem with pruning may be an underlying cause, explaining why children with ADHD often have other mental health conditions too. Ultimately, it leads to delayed development of the prefrontal cortex, which is responsible for the “cognitive control” we have over our emotions and behaviour. That means people with ADHD can struggle with their emotions.
Delayed development of the prefrontal cortex may also explain why children with ADHD often have cognitive deficits, such as problems with executive functions (for example planning, self-monitoring, self-control and working memory). But then, so do children with depression and anxiety. So which is ultimately the root of the problem?
One recent and large study of 11,876 children, aged 9-12, provides a clue. At the University of Cambridge, we found that the cognitive deficits in children with more ADHD symptoms were related specifically to problems with attention, rather than emotions.
Children with anxiety and depression symptoms only exhibited those deficits if they also had problems with attention. So it seems that one possible route to helping children with ADHD or mood disorders with cognitive development is to focus on improving their attention.
Treatments
Another way to learn more about ADHD is by studying the effects of the drugs used to treat it. The main pharmacological treatment for ADHD is called methylphenidate, or Ritalin.
Methylphenidate roughly works by increasing three chemicals in the brain: dopamine, serotonin and noradrenaline. Dopamine can improve attention, learning, working memory and motivation, while noradrenaline reduces impulsivity and boosts attention. Serotonin is known to improve symptoms of anxiety and depression.
We know a considerable amount about which areas of the brain these drugs target. Indeed, the dopamine system affects multiple brain regions.
One study showed that attention was improved by methylphenidate treatment and that this was associated with increases in dopamine in the brain’s ventral striatum (a region involved with reward and motivation). This means the dopamine reward/motivation circuit in the brain is probably important in ADHD.
Another study showed that methylphenidate improved working memory, which is known to be affected by dopamine, and showed increased blood flow to the prefrontal and parietal cortices –important areas for executive function. This research suggests that cognitive control, which is associated with frontal areas, can be improved by methylphenidate.
It also backs up our finding that ADHD is linked to delayed development of the prefrontal cortex, making it harder to exert cognitive control.
Similarly, a further study showed that methylphenidate significantly improved emotional symptoms in adults with ADHD. But we still don’t know whether methylphenidate is working to control emotion in a top-down way through the prefrontal cortex, or whether it is working directly on emotion processing itself, or a combination of both.
That said, it is now becoming clearer that a problem with regulating emotions is a core symptom of ADHD, and not simply a co-occurring issue. As such, emotional dysregulation is an important target for treatment.
Cognitive behavioural therapy is effective in treating problems of self-control and low mood. This should be offered to children with ADHD, in conjunction with pharmacological treatments.
ADHD on the rise
The number of ADHD diagnoses are rising across the world, and so are prescriptions of methylphenidate. Indeed, according to the National Health Interview Survey, the prevalence of diagnosed ADHD among children and adolescents aged four to 17 in the past 20 years have increased from 6.1% to 10.2% in the US.
In the UK, a study estimated that the use of ADHD medications has increased by almost 800% from 2000 to 2015.
With the increasing use of technology and remote school and work, we are multi-tasking and splitting our attention, rather than focusing it on one task at a time, more than ever. It may be that the prevalence of ADHD will increase even more in the future as coping strategies become less effective and people seek help and ultimately receive a diagnosis.
Ironically, some of the solutions may rely on technology, such as cognitive training using game apps on an iPad or mobile phones, for example Decoder, which has been shown to improve attention in young adults.
The more we learn about brain basis of ADHD, the easier it will get to treat.
Barbara Jacquelyn Sahakian receives funding from the Leverhulme Trust and the Lundbeck Foundation. Her research work is conducted within the NIHR Cambridge Biomedical Research Centre (BRC) Mental Health and Neurodegeneration Themes and the NIHR MedTech and in vitro diagnostic Co-operative (MIC). She consults for Cambridge Cognition. Cambridge Enterprise has technology transferred Decoder to PEAK and PopReach. She receives royalties from PopReach.
Christelle Langley is funded by the Leverhulme Trust. Her research work is conducted within the NIHR Cambridge Biomedical Research Centre (BRC) Mental Health and Neurodegeneration Themes and the NIHR MedTech and in vitro diagnostic Co-operative (MIC).
This article was originally published on The Conversation. Read the original article.

.jpg?w=600)





