You may have heard reports in recent days of a “flesh-eating bacteria” spreading in Japan, referring to an illness that can occur with streptococcal toxic shock syndrome (STSS).
Media reports indicate the country has seen more than 1,000 cases of STSS in the first six months of 2024, more than the total for all of 2023. However, these cases have not yet been published in peer-reviewed journals, so reports may not be entirely accurate.
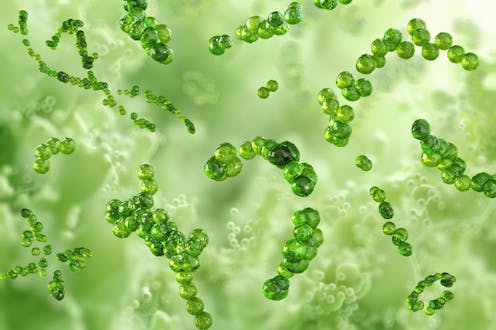
STSS is caused by Streptococcus pyogenes bacteria, or “Strep A”. These bacteria are quite common, but certain strains can cause more serious illness – called invasive group A streptococcal disease.
Since 2022, many countries, including Australia, the United States, and countries in Europe, have noted a rise in severe invasive group A streptococcal disease. This surge is part of an overall increase in Strep A infections.
So what is STSS, why is it surging now, and is it cause for concern?
Who gets STSS?
At any time, many people will be “colonised” with Strep A, meaning the bacteria is living harmlessly in their throat or on their skin.
Strep A also causes sore throats (“strep throat”) and skin infections. Sometimes, for reasons that still aren’t entirely clear, Strep A causes invasive infections like pneumonia, nasty “flesh-eating” skin infections, and STSS. In these ways, Strep A is an important cause of sepsis, a term which broadly refers to a life-threatening infection.
STSS is the most severe Strep A disease, though fortunately it’s really rare. It mostly affects young children and the elderly but cases do occur at all ages. Pregnant people may also be at higher risk, including soon after delivery.
What are the symptoms?
In STSS, the bacteria produces a toxin that can result in an overwhelming immune response in some people.
The illness can progress to become life-threatening in a matter of hours and has a high mortality rate – up to 40% of people who develop STSS will die.
However, the early signs and symptoms of STSS can overlap with common viral illnesses, particularly in children, making it hard to diagnose.

Symptoms are vague in early invasive group A streptococcal infections – things like fever, rash and nausea. But it’s important to look out for signs of sepsis, which suggests something more serious might be going on.
Signs of more severe invasive group A streptococcal disease, including STSS, are similar to those seen in other bacterial causes of sepsis (such as meningococcal disease). These include lethargy (drowsiness), fast breathing, a rapidly changing rash, aching muscles and confusion.
STSS sometimes co-occurs with a condition called necrotizing fasciitis, also caused by Strep A, which is the “flesh-eating” presentation of the infection. This is when the skin cells die in response to the toxins produced by the bacteria.
Parents of young children should trust their gut. If you’re worried your child is sicker than they usually would be with a common bug, and particularly if they have cold limbs, a red rash (like sunburn), or are less responsive, seek medical attention quickly at your nearest emergency department.
Why now?
Studies suggest certain more virulent strains of Strep A might be one part of the current STSS surge.
Also, in 2020–21, at the height of the COVID pandemic, when there was less close contact between people, there was likewise less exposure to Strep A (and other bacteria and viruses). For younger children especially, that meant they didn’t build up the partial protection against bad Strep A infections that comes from repeated exposure.
With more human contact from 2022 onward, there has been more transmission of Strep A, with children more vulnerable to contracting more severe disease, including STSS.
This is not unique to Japan. Although rare, we’ve seen many cases of STSS in Australia and elsewhere.

How is STSS treated, and can we prevent it?
Strep A can be killed by penicillin, one of the oldest and most widely available antibiotics. When STSS is diagnosed early, antibiotics usually prevent most serious complications.
Other medicines, like immunoglobulin, might be required to put the brakes on an out-of-control immune response, and patients often need support in an intensive care unit.
There’s no vaccine to prevent STSS and other Strep A infections (unlike other bacteria like meningococcus and pneumococcus, which are in the national childhood immunisation program).
Researchers in Australia and around the world are working hard to try to find a vaccine to prevent Strep A infections.
Serious Strep A infections like STSS often follow viral infections, especially chickenpox and influenza, so staying up to date with vaccines in the national schedule (which includes chickenpox), and ensuring you receive the seasonal influenza vaccine, reduces the risk.
Strep A can be spread via large respiratory droplets or direct contact with infected people or carriers. Simple hygiene measures (like hand washing and covering your cough) reduce the amount of Strep A circulating in the community.
Planning a trip to Japan? There’s no need to cancel your holiday
STSS is a rare but serious complication of Strep A infections, which can occur in humans anywhere. So, unless you’re trekking alone to the South Pole, you’re at a very similar (and very low) risk of contracting a serious infection.
Make sure you’re up to date with immunisations including the seasonal flu vaccine. Always practice good hand hygiene, and remember the signs of severe bacterial infections that require urgent medical attention.
Phoebe Williams receives funding from The National Health and Medical Research Council.
Joshua Osowicki receives funding from the Australian National Health and Medical Research Council, the National Institute of Allergy and Infectious Diseases of the United States National Institutes of Health, and the Leducq Foundation.
Yara-Natalie Abo receives funding from the National Health and Medical Research Council and the National Heart Foundation.
This article was originally published on The Conversation. Read the original article.







