The head and the heart are often positioned as dueling facets of our being. When faced with a challenge, do you follow your heart or your head?
But positioning the head and heart in opposition to one another is to ignore a vital (and just as poetic) truth: The head and the heart are a team.
While doctors once thought the link between mental health and heart health was likely limited to vague, negative emotions to do with lifestyle choices, experts today understand that there is a bidirectional relationship between mental health and heart health. People with mental health issues have a higher risk of heart problems and vice versa.
Now, we know that heart health and mental health are closely linked — but we don’t know exactly why. But scientists are trying to find out.
What’s new — In a recent review of 12 studies published in the journal BioMedical Engineering Online, scientists found that people with anxiety, depression, and panic disorders are more likely to experience poor heart health, regardless of their age.
“Decreasing stress and anxiety levels are ways to take better care of heart health.”
But poor heart health is not an inevitability for those experiencing mental health issues. Instead, these results reinforce the importance of “early therapeutic intervention” for these brain conditions, the study authors write.
Beyond therapy, maintaining one’s general health is also critical, co-author Renly Lim tells me. Lim is a research fellow at the University of South Australia. This includes maintaining a healthy diet, exercising, and getting enough sleep.
In turn, taking care of your mental health is a great way to take care of your heart, Lim explains.
“Talk to your health professional to discuss your options — both non-medication and medication treatments, as well as lifestyle changes — to better manage any mental health problems,” Lim says.
“Decreasing stress and anxiety levels are ways to take better care of heart health.”
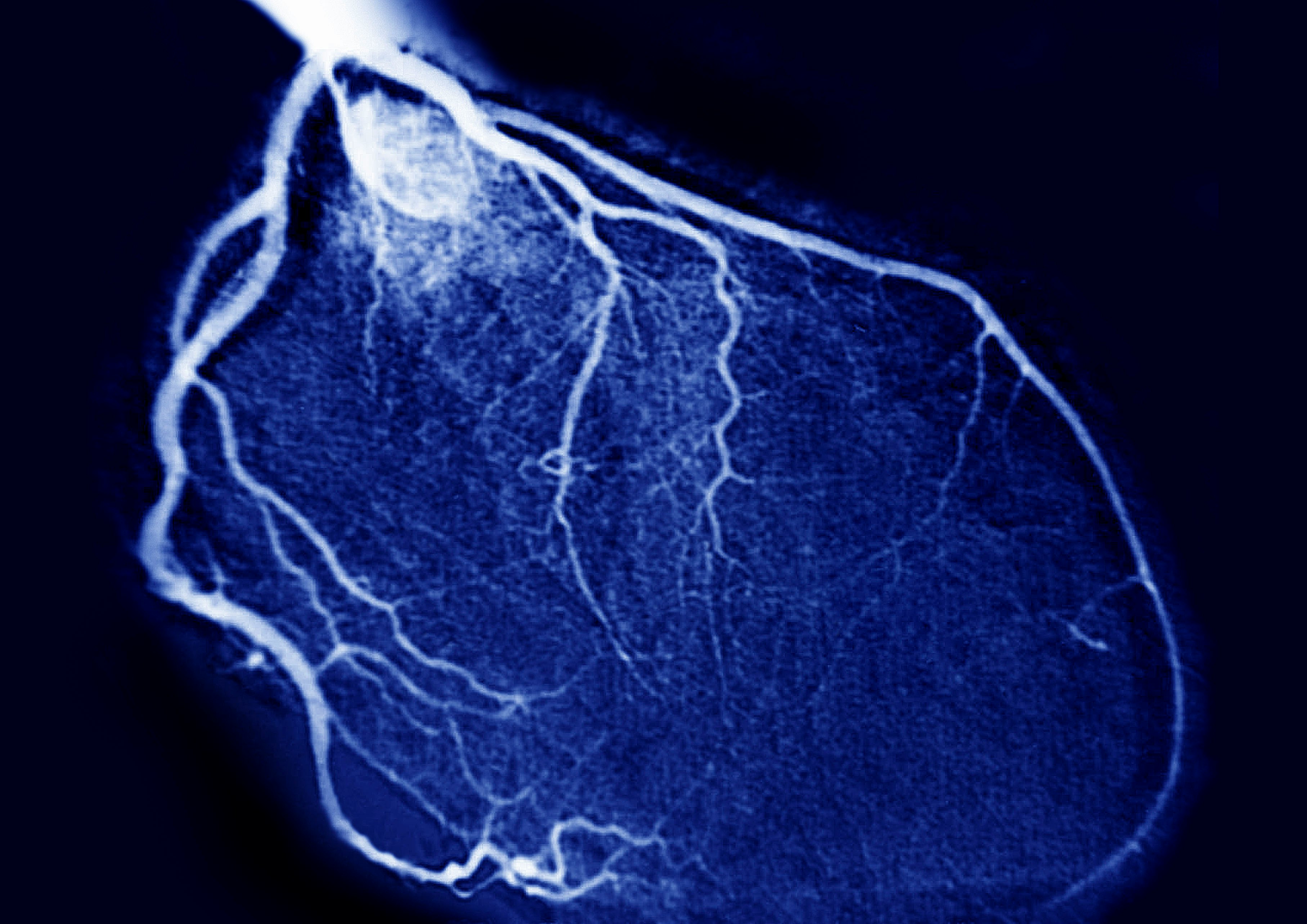
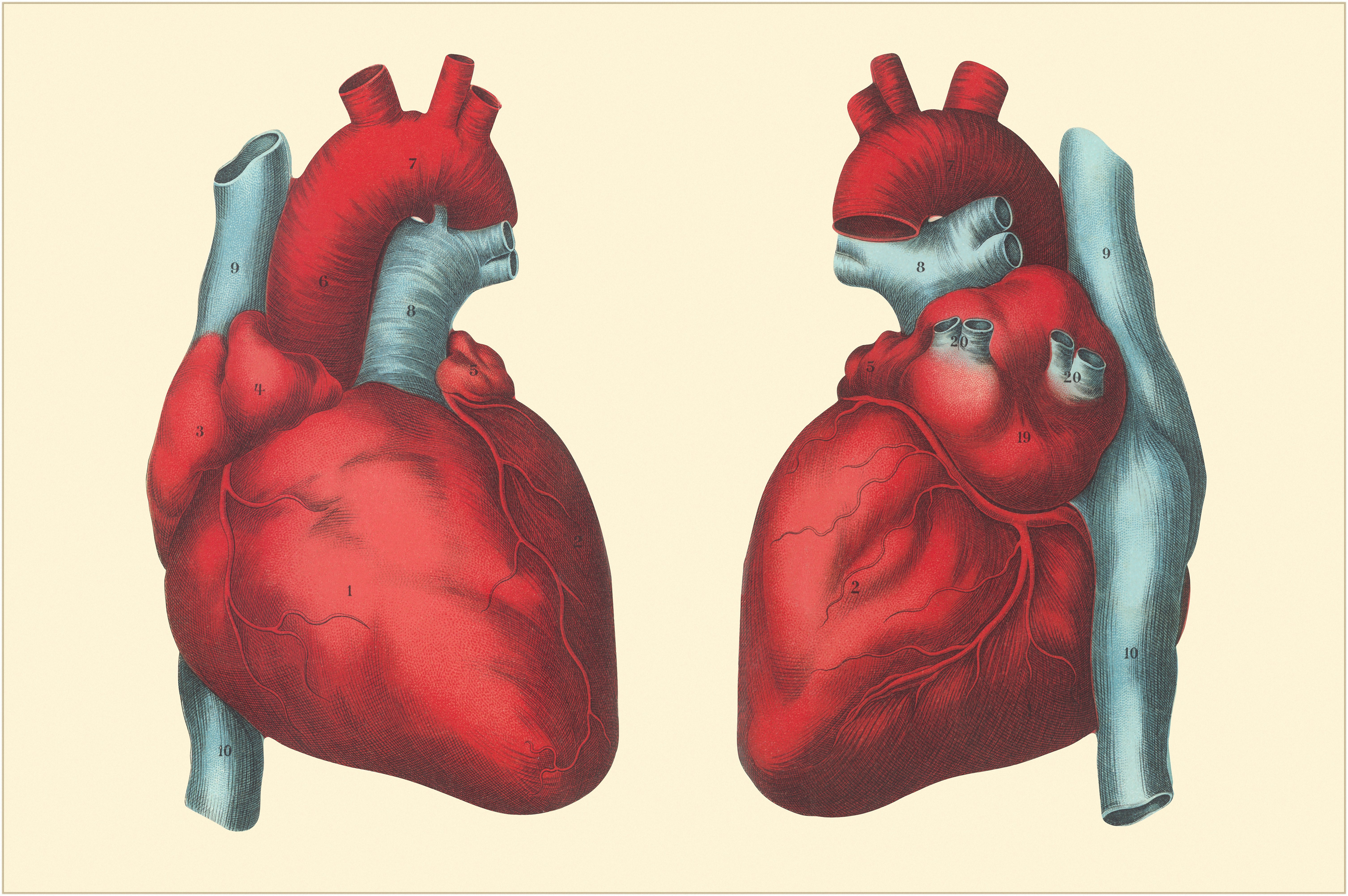
How they did it — Lim and her colleagues’ review pays particular attention to blood pressure variation and heart rate variation (HRV). Unlike heart rate, which is how many times a heart beats in a minute, HRV measures the time between two heartbeats. A constantly changing HRV is a sign of good health — it suggests the body is adapting to external stressors. Scientists discovered that people with mental health problems are more likely to display reduced HRV.
“Low heart rate variation occurs when our body is in fight-or-flight mode,” Lim explains.
“People with mental health problems could have reduced HRV because they are less adaptable to external stressors.”
This lack of adaptability suggests the body remains in a state where it senses danger. Low HRV is also common in people with chronic diseases.
The review also suggests people who experience poor mental health are less likely to show typical patterns of rising and falling blood pressure throughout the day. While spikes in blood pressure aren’t healthy, it is healthy for systolic pressure to dip between 10 and 20 percent at night. This allows the heart to rest. However, people with mental health problems are more likely to experience dips under 10 percent.
Why it matters — “These findings may have important implications for patients’ future physical health and well-being, highlighting the need for comprehensive cardiovascular risk reduction,” the study team writes.
Of all physical conditions, cardiovascular disease is the most common cause of death among people with mental illness.
While researchers work toward understanding the precise nature of the link between heart health and mental health, it’s critical for individuals to consider this mind-body connection — and for care providers to do what they can to provide the necessary support.







