
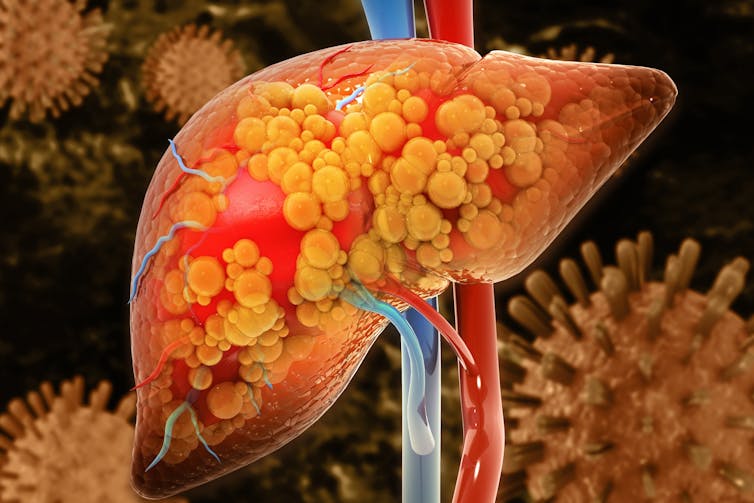
Around 2% of adults worldwide suffer from a condition called non-alcoholic steatohepatitis (Nash), an advanced form of non-alcoholic fatty liver disease. This occurs when fat builds up in the liver, causing inflammation and scarring.
Without treatment it can eventually lead to liver cirrhosis – and it can also increase the risk of other serious health conditions, such as heart disease.
There is currently no medication to treat Nash. Since excess fat in the liver is what causes the inflammation and scarring that is characteristic of the condition, the current mainstay treatment for patients is weight loss.
However, the kind of weight loss most people are able to achieve on their own is modest and not enough for significant reductions in liver fat and change inflammation and scarring.
But our recent study has shown that rapid weight loss achieved through the “soups and shakes” diet – which is commonly used to treat obesity and type 2 diabetes – may be able to reduce the severity of Nash.
To conduct our study, we recruited 16 participants with obesity, Nash and moderate to advanced liver scarring. Five of the participants were female and 11 were male. Most participants were white.
All of the participants took part in the “soups and shakes” weight loss programme, replacing their regular meals with specially formulated soups, shakes and bars for 12 weeks. They consumed four products of their choice daily, which provided them with about 880 calories and all the essential vitamins and minerals.
After the initial 12-week period, they gradually began re-introducing regular food to their diet over the next 12 weeks. They were also given regular support from a dietitian to keep them on track and motivated throughout the 24-week study.
At the start of the study, participants were weighed, had their blood pressure taken, blood tests done and two scans that measured the health of their liver. These scans estimated how advanced their liver inflammation and scarring was and the amount of fat in their liver.
These tests were also repeated at 12 and 24 weeks – with an additional blood test done at four weeks.
Fourteen of the participants completed the 24-week study. Participants lost an average of 15% of their body weight, showing they largely adhered to the weight loss programme.
Our study also showed that the rapid weight loss was safe for participants. In the past, this kind of diet programme wasn’t recommended to Nash patients due to concerns over how safe it may be. The most common side effect patients experienced was constipation – but this was temporary and typically only mild.
Scans also showed that most participants had significant improvements in liver fat and in markers of liver inflammation and scarring.
Bigger improvements than medication
These are some of the largest improvements in liver disease severity reported in research to date, approaching the level of improvement seen with weight loss after bariatric surgery. No trialled medication has shown such a large improvement.
While some weight regain is likely to happen, if participants are able to maintain at least most of their weight loss after the study ends, this could possibly reverse the trajectory of their liver disease.
What’s more, systolic blood pressure and haemoglobin A1C (a marker of blood sugar control) also significantly improved in participants who’d had hypertension and type 2 diabetes at the start of the study. This may suggest that the programme could be used to reduce the risk of heart disease, which is the most common cause of death in people with Nash.
Because our results are only from a small study, further research is needed to test this programme in a larger trial with more diverse participants and a control group. It will also be interesting to see whether this programme could be useful for patients suffering with more advanced forms of liver disease – such as liver cirrhosis.
But it is promising to see from our study that the diet appears to be safe for people with Nash and effective in improving their liver health.
Dimitrios Koutoukidis receives funding from National Institute of Health Research. The intervention was donated to the University of Oxford by Nestle Health Science with dietetic support provided by Oviva. Perspectum donated the MRI analysis. None of these associations led to payments to the author.
This article was originally published on The Conversation. Read the original article.





