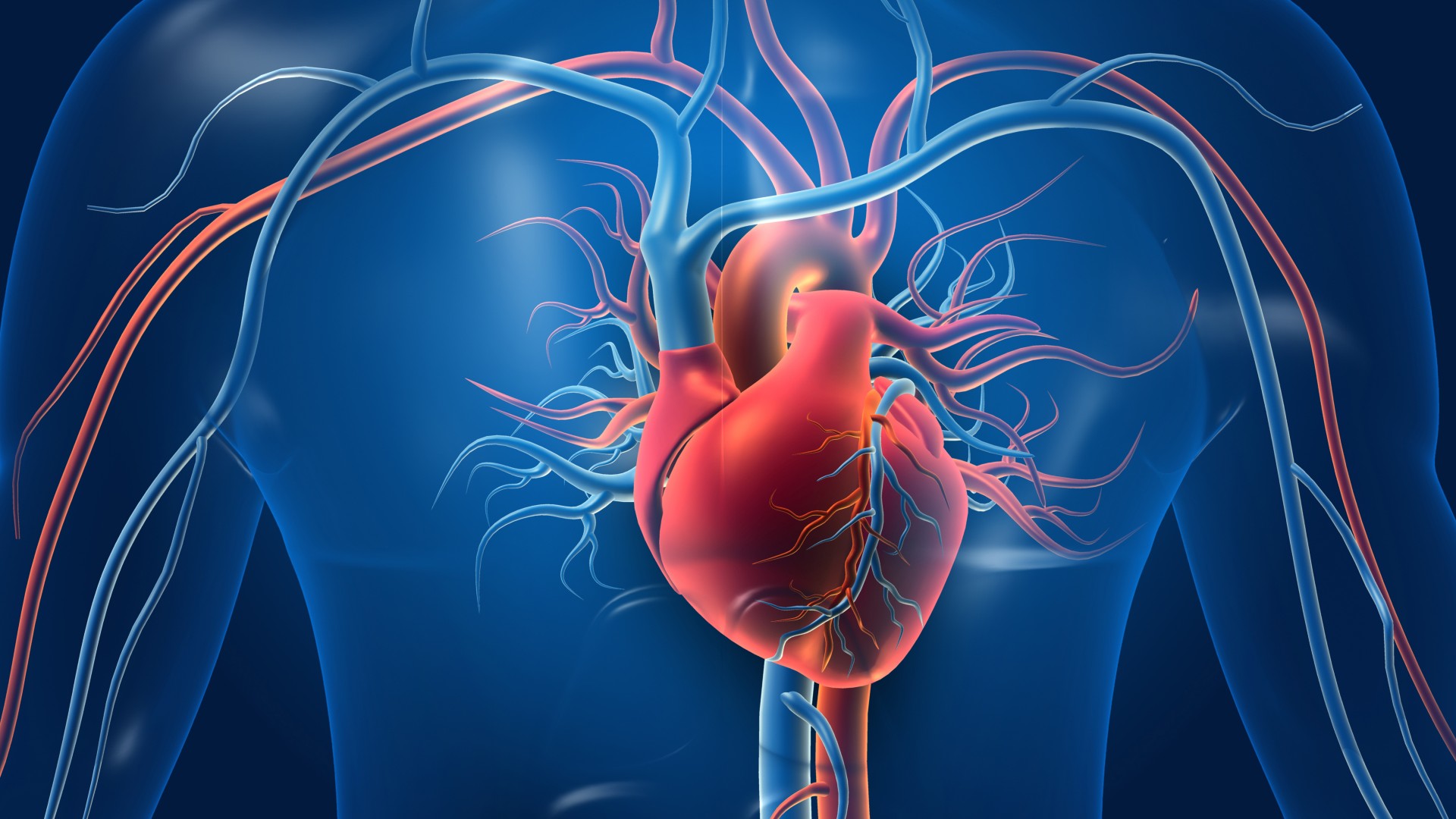
Coronary artery disease (CAD) is the most common type of heart disease and occurs when plaque buildup narrows or blocks one or more of the arteries that supply blood to the heart. The term is often used interchangeably with coronary heart disease (CHD).
Specifically, CAD is a problem of one or more arteries supplying the myocardium, the muscular layer of the heart. This is the thickest layer of tissue in the organ and consumes more oxygen than the rest of the heart, consequently requiring the most blood flow.
According to the Centers for Disease Control and Prevention (CDC), 382,820 people in the United States died from CAD in 2020, while 20.1 million adults ages 20 and older live with the condition.
What causes coronary artery disease?
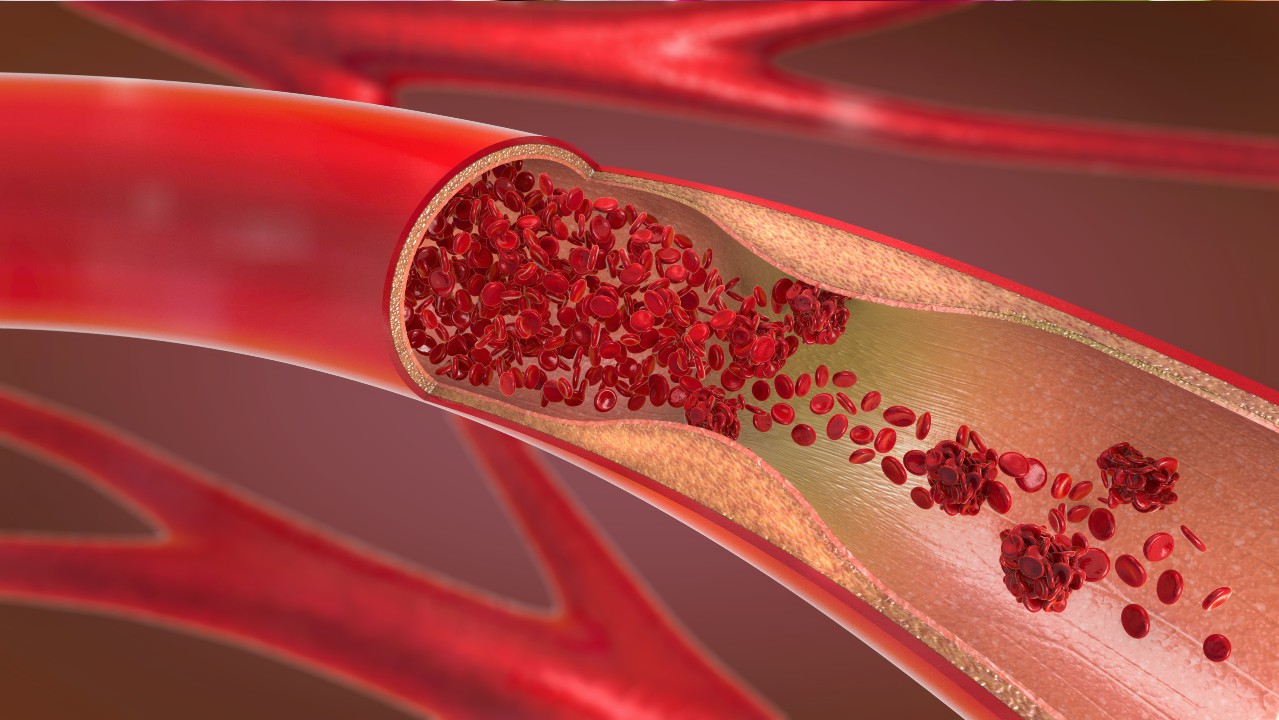
CAD is caused by a process known as atherosclerosis, in which plaque builds up in the inner walls of arteries, causing them to narrow and become rigid. This blocks blood flow, and the blockage can rapidly worsen if a piece of plaque breaks off and causes a blood clot.
One factor that increases the likelihood of atherosclerosis is the long-term presence of high concentrations of low-density lipoprotein (LDL) cholesterol in the blood. These high levels can result from a relative deficiency of LDL receptors, which are proteins on the membranes of various body cells, especially liver cells. LDL receptors capture LDL from the blood, causing its contents — cholesterol and fat molecules called triglycerides — to be taken inside the cell and out of the blood. Thus, a lack of these receptors causes LDL cholesterol levels to be higher in the blood.
High levels of LDL cholesterol provoke and exacerbate what doctors call atherosclerotic cardiovascular disease, an umbrella term for atherosclerotic changes that can develop in blood vessels throughout the body; this includes CAD, which specifically affects the coronary arteries.
Other factors that can provoke atherosclerosis include uncontrolled type 2 diabetes, hypertension (high blood pressure) and tobacco use.
What are the symptoms of coronary artery disease?

Symptoms of coronary artery disease generally don't appear until the narrowing and hardening of coronary arteries begins to obstruct the flow of blood to the myocardium (the muscular layer of the heart).
When this obstruction does occur, it can produce angina — chest pain or chest heaviness that arises when the heart doesn't get enough oxygen — as well as pain in other places, such as the neck, shoulder or arm. Angina can be stable at first, meaning that it generally occurs only with exertion, related to physical activity or emotional stress and the strength of each heart contraction. However, this can progress to unstable angina, which is a type of acute coronary syndrome (ACS), a range of conditions associated with sudden, reduced blood flow to a part of the heart.
Known colloquially as a "heart attack," ACS is a spectrum running from its least severe subtype, unstable angina; to an intermediate subtype, non-ST elevation myocardial infarction (NSTEMI); to its most severe subtype, ST elevation myocardial infarction (STEMI).
According to the Mayo Clinic, symptoms of ACS resulting from coronary artery disease may include:
- Dyspnea (difficulty breathing or shortness of breath)
- Chest pain or chest heaviness
- Pain in other places, such as the neck, shoulder or arm
- Fatigue
- Palpitations
- Dizziness or fainting
- Nausea
- Sudden sweating
How is coronary artery disease diagnosed?

To diagnose coronary artery disease, doctors will look at a patient's medical history and any symptoms that could indicate heart problems. They may also perform a physical examination.
Often, they will request an electrocardiography (ECG) test. ECG is a technique that detects changes in voltage over time across the heart, at different angles. When CAD causes enough blockage of blood flow to cause ischemia (insufficient blood supply) in particular parts of the heart, ECG can show abnormalities in the heart's activity.
Doctors also will request blood tests. Important blood values include the concentration of LDL cholesterol in a person's blood and the concentration of triglycerides (fat molecules).
Patients may be referred to a cardiologist for further tests, such as additional ECG testing, ultrasound imaging of the heart (echocardiography), or evaluation with a wearable heart monitor, a version of ECG that you wear for a few days or weeks that transmits data to the cardiologist.
Complications of coronary artery disease
Coronary artery disease can lead to a condition called myocardial ischemia in which an artery cannot deliver adequate quantities of blood and oxygen to the myocardium. This can happen due to an artery gradually becoming blocked with plaque, resulting in the lumen of the artery (the hollow middle through which blood passes) narrowing and the wall of the artery hardening.
In addition, an atherosclerotic artery that has not been blocked enough to cause ischemia can suddenly become blocked by a piece of plaque breaking off, getting stuck and growing larger by stimulating the clotting process. Generally, this would lead to ACS.

Even without a plaque rupture, however, the gradual increase in blockage driven by atherosclerosis disrupts a person's ability to perform physical activities, such as walking up stairs or around the block.
When doctors suspect that a patient's CAD may be causing life-threatening problems with the heart, such as ACS, myocarditis (inflammation of the heart's muscular tissue) or pericarditis (inflammation of the sac surrounding the heart), blood is tested to see if levels of certain enzymes are elevated, including a group of enzymes called troponins. Troponins are measured because they leak out of heart muscle tissue when it is damaged.
In cases of ACS, doctors can use troponin measurements and ECG to distinguish between broad subtypes of ACS, which has important implications for treatment and further testing. In cases when either heart failure or myocarditis is suspected, they'll also check blood for levels of brain natriuretic peptide (BNP), a hormone that enters the blood when the heart is stressed.
Treatment for coronary artery disease
Treatment for CAD usually involves a combination of medication and lifestyle changes.
Medications can include cholesterol-lowering drugs, aspirin (to make it harder for platelets to stick to one another and to walls of blood vessels to form clots), medications to slow the heart while increasing the power of each contraction, or medications to widen blood vessels and/or to decrease blood pressure.
Lifestyle changes can also help to reduce a patient's risk of CAD and related health problems. According to the Cleveland Clinic, these include stopping smoking, limiting alcohol use, maintaining a healthy weight, limiting foods high in saturated fat, sodium and sugar, and getting enough sleep.







