Rose learned there was an outbreak in her aged care home in New South Wales when “an enormous man” she had never seen before stood over her bed and woke her up at midnight.
“He was all dressed in PPE and said, ‘you have to have a rapid antigen test [RAT] – we’ve got a case of Covid in the home’,” the 81-year-old says.
“It was quite a shock. When he left I pulled the sheet over my head. I could hear other residents crying because they would have been very frightened to have been woken like that. It wasn’t very well handled. I think the staff panicked.”
Since the highly infectious Omicron strain of Covid-19 emerged in Australia in late November, the virus has spread through aged care like wildfire.
In January, 499 aged care residents died with Covid-19, more than the total number who died in Australia in 2021. Most deaths were in New South Wales. In February so far another 34 aged care deaths have been reported, bringing the total in 2022 to 533. There were 685 aged care deaths in the whole of 2020.
Currently, 1,176 aged care facilities are battling an active outbreak. Most are in NSW (525 homes), followed by Victoria (275), Queensland (202) and South Australia (137). Across the country, 11,980 aged care residents and staff had an active case on 4 February.
Two years into the pandemic many residents and staff at affected homes report dangerous staff shortages, with cleaners and lifestyle workers being called on to handle personal care and food preparation roles outside their skillset. On Friday, the defence minister, Peter Dutton, raised the prospect of troops being sent in.
Residents and staff in different locations have told Guardian Australia that when an outbreak occurs, many homes panic and seem unsure of their own plans.
Some residents are immediately locked down, meaning they are unable to see family and friends for weeks. Different homes have had different policies on visits throughout the Omicron wave, even when there is no active outbreak.
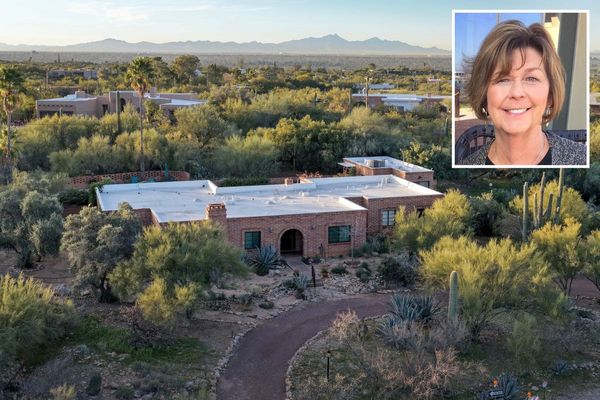
The home where Rose lives was in lockdown from mid-January to early February. She was not allowed outside for fresh air but was permitted to go to the cafe under supervision for one hour in the mornings to read the sport news from the paper for a friend and fellow resident who is blind.

“My granddaughter wanted to come to the glass front door and just wave to me,” Rose says. “That wasn’t permitted sadly. And so all I can say is thank goodness for the internet. But not all residents can use the internet and [they] are just sitting in their rooms watching television 24/7. I think the lack of communication would be most sorely felt by them.”
Rose makes it clear she does not blame staff for the way the outbreak was handled and that they showed care and compassion – but she is baffled by the lack of government support for them.
“A lot of staff have been off sick of course, and the outside staff [such as gardeners and maintenance staff] have been filling in doing a magnificent job, not with personal care, but with delivering meals and helping with the laundry, all that sort of thing. But I think the government’s been really lacking, and a lot more could have been done sooner. I think the aged care minister, Richard Colbeck, is an absolute disgrace. I mean going to the cricket … what are his priorities, really? Does he know what’s going on?”
The nursing manager of the home where Rose lives says she based her outbreak management plan on the federal government’s Covid support plan for aged care, which promised a surge workforce in times of outbreak. But when the home experienced its outbreak and she desperately needed extra staff, “there was no surge workforce,” she said. “I didn’t get a single additional staff member.”
Now that the outbreak is over, the PPE supplied by the federal government has started to arrive. The home managed only because the nursing manager “hoarded and locked up PPE I found myself for the past two years in preparation for this”, she says.
“I wasn’t going to rely on the government to supply it,” she says. “No way. Now it’s arriving of course, and I have 20,000 gowns I don’t know what to do with. But we may have another outbreak, so I will keep them.”
The nursing manager says the outbreak began when three staff members working in the same section of the home tested positive within 32 hours, so she made the call to send staff in that same night to test those residents at the highest risk of being exposed. She says she believes residents were woken up closer to 10pm than midnight.
“But it wasn’t ideal,” she says. “However, I made that call because I didn’t want any staff going in to help a resident throughout the night and then spreading it. It was also the advice the public health unit gave me.
“I am close to retirement and I have managed hospitals, worked in intensive care and acute care … and I have never felt pressure like this. I am proud that where I work now, I have had one of the highest retention rates of my staff in the industry. But not now – not since Omicron hit. The reality is, this government has made a huge amount of mistakes. My staff should not be on the pittance they are being paid. I don’t think anyone in aged care is OK.”
‘I feel helpless’
According to the public health researcher and director of Aged Care Matters, Dr Sarah Russell, the federal government has a “hands-off approach”, treating each aged care home as an individual business.
“As a result, many federal aged care homes are a law unto themselves,” she says. There are inconsistent and sometimes inhumane policies around visits, Russell says, as well as different policies on staff ratios.
In state-run care homes the rules are different again. Victorian-owned public aged care homes, for example, operate under the Safe Patient Care Act, which prescribes ratios of registered nurses.
“On the morning shift, one registered nurse is required for every seven residents; in the afternoon, one registered nurse for every eight residents; and on the night shift, one registered nurse for every 15 residents,” Russell says.
“Compare this with staffing in privately-owned residential aged care homes, where a single registered nurse is often required to look after more than 100 residents. Not surprisingly, deaths in aged care homes during the current outbreak in Victoria are almost exclusively a private sector aged-care issue. And all residents in Victoria-owned aged care homes were offered a booster before Christmas.”
Of the 46 aged care deaths in Victoria during the Omicron outbreak to 31 January, just four were in state-run care homes.
Jess, who works in a private aged care home in Sydney, says the facility “makes up their own rules”. A lifestyle worker, her role is to facilitate outings and activities for the residents. Instead, with Omicron spreading through the home, she has found herself working as a personal care worker, bathing residents and feeding them.
“I showed up to one shift and there was just one carer per 45 residents and they only managed to find one relief staff member,” she says.
“It was awful. The manager told me I had to work the floor doing caring and feeding, even though I’ve never been trained in all the things that carers are taught how to do. Then the residents are just asking us constantly, ‘When can I go out?’, ‘When can I leave my room?’, ‘When can I see my family?’. They are just devastated.”
Jess says she has seen people still in bed at 1pm because they need two staff members to help them out or into a wheelchair – but there are no staff free.
“I feel helpless because I can’t lift them and haven’t been trained to use a hoist,” Jess says. “In the last three weeks especially, they’re yelling out for help. I have noticed their buzzers to call for assistance are being turned off by the staff, or moved just out of reach for them.
“Everyone’s just calling and calling for the nurse but if they’ve got two nurses it’s just physically impossible for everyone to be seen. But I have plugged a few buzzers back in or moved their bedpan close enough to reach.
“One of the worst situations I saw was a lady with quite severe dementia, and she was sitting in her own poo and urine. I went and tried to get the nurse but there were only two nurses on that day, and they needed two people to use the hoist machine. And so this poor lady had to wait until they were both available. It just took forever and this lady had to sit in her own poo, which had also gone all over the floor. It was an infection risk and a slip risk and I was just thinking: this is a fucking nightmare.”
‘I’m going to work every day with anxiety’
An assistant nurse working in an aged care facility in Newcastle, NSW, says personal care, such as showers, is the first thing to suffer during staff shortages. There is also no time to talk with residents or take them outside.
“When you’ve only got four staff you have to prioritise,” she says.
“It means Betty down in room 204 might have to go without a shower. Safety, administering medication, watching dementia patients and preventing them from wandering and falling all have to come first. It’s not fair, because for some people, a shower is the only thing they have to look forward to.
“Just in the past month, those hard choices have really had to be made. Yes, staffing was challenging before, but we were able to still provide personal care. The government is letting us all down with a lack of resources and support.”
She says she loves her work, but the Omicron outbreak has compelled her to leave the industry.
“Usually, at full staff for 256 residents, we would have two registered nurses, an enrolled nurse, and between seven to 10 staff on the floor,” she says. “Lately we have one registered nurse, often an agency nurse who doesn’t know the residents, and five or fewer staff on the floor. Up to 60% of our staff on any shift are wiped out. I get text messages every day from the person doing rosters saying they urgently need at least five people … it’s exhausting. I feel like I’m deserting my residents”.
The final straw, she says, was when she was left managing the facility one night due to staff shortages – even though she is only qualified to work as an assistant nurse responsible for personal care.
“The residents are like family to me and leaving is the hardest decision I’ve ever had to make,” she says. “But I’m going to work every day with anxiety thinking, ‘what am I going to be faced with today and how am I going to get through my shift?’. I’ve been placed in positions that I should never have been placed in since Omicron hit.”

The only way to improve the situation is to make aged care more specialised, requiring a higher level of training and education nationally, and to increase pay substantially to reflect that training, the nurse says. She is angry that two years into the pandemic this is not happening.
“We don’t just need more staff, we need the right staff,” she says. “When I did my course five years ago, 40% of the people that were there didn’t really want to do it. One of the questions we were asked was: ‘what would you do to make a person with dementia’s day better?’ And one person responded: ‘why would you bother to try since they don’t even remember anything anyway?’
“We need to make sure we’re attracting quality people who really want to be there and improving the level of education and pay is key to achieving that.”
Couldn’t find their father in his room
Amid growing unrest among staff, the prime minister, Scott Morrison, announced on Monday that aged care workers would receive two pre-election bonus payments worth up to $800. The Health Services Union was scathing, describing it as “too little, too late” and inadequate to address gross underpayment spanning years.
Meanwhile, family members of residents have taken to social media to share their stories, and have expressed anger at the deaths being described as in people who were “palliative” by the time they got Covid. Compiling experiences from a dementia unit in Victoria, one person described finding their father “swimming in faeces”. Another person couldn’t find their father in his room, only to discover he was “sitting asleep in the shower chair in the bathroom of another resident’s room”.
The federal minister for aged care services, Richard Colbeck, told Guardian Australia the Omicron variant, combined with continued circulation of the Delta variant, was “significantly impacting the residential aged care sector”.
But he says the spread in aged care was being driven by community transmission and not through a lack of aged care resources. He denied there was a lack of booster shots being administered or poor infection control.
“The strongest predictor of cases in aged care are high case numbers in the community – through staff exposures in the community, residents leaving the facility and visitors entering,” Colbeck said.
“There has been an unprecedented increase in outbreaks in facilities over the last month, driven by significant increases in cases in the community. Each outbreak has different factors that impact the risk of transmission on site.”
But Russell rejects this assessment.
“He always uses community transmission as an excuse,” Russell says. “His job is to protect residents in the face of community transmission. The way to do that is to get people their booster shots and get rapid antigen tests and staff before they [governments] let it rip.”
‘The last straw’
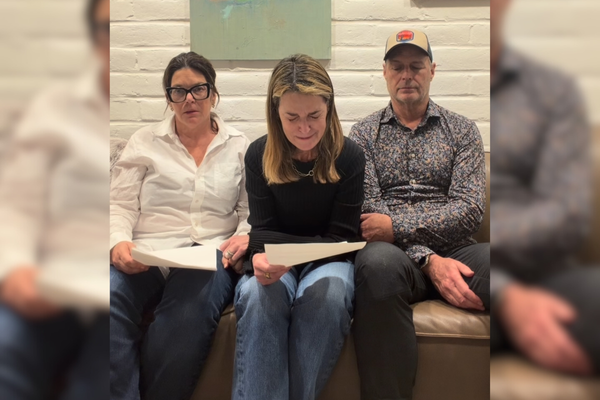
Carolyn Smith is the national aged care director for the United Workers Union, which represents workers in aged care. The latest outbreaks – and deaths – were evidence that aged care homes were unprepared and abandoned by the government to “fend for themselves”, she says.
“Workers have told us there is no visible surge workforce, the booster program has been a shambles, many facilities lack even the most basic PPE, and RAT tests have not been available.”
Queensland aged care worker Mandy says none of the staff where she works were RAT-tested, despite an Omicron outbreak in the home.
“Rumour has it that some are coming in – everything is rumour,” she says. Meanwhile double shifts are being regularly requested.
“You almost feel like you are coerced into doing them … I said I can’t leave my dog 16 hours so they said I could have my dog on site for the second shift. There are no signs of a surge workforce.
“We have no cleaner, we have no cook. I worked my day off as a cook. I’m not trained as a cook – it’s that desperate.”
She says staff were made to work between parts of the facility with Covid-positive and Covid-negative residents – and that at the start of the outbreak there was confusion when it came to donning and doffing PPE.
“N95 masks didn’t start coming out until staff and residents began getting sick – so too late,” she says.
Prof Nigel McMillan, the head of infectious diseases from the Menzies Health Institute in Queensland, says N95 masks are the only type that should be used by aged care workers during the Omicron outbreak.
“N95 are well known to be the most effective, and surgical or cloth masks are not going to do a good job,” he says.
Mandy says while staff struggled, isolated residents suffered the most.
“We had one dementia resident [in isolation in their room] who had no TV, radio, nothing,” she says.
“Frustrated, angry residents see it as being our fault they are locked up. I care. Who is going to look after these people if we don’t? But we’re an ageing workforce. I’m 58. Half our staff are over 50. And plenty are getting to the point where this is the last straw.”