
Warning: This article contains graphic images.
Xylazine or “tranq” wounds – characterized by deep pockets of dead tissue – have become increasingly visible in Philadelphia among people who use drugs.
That’s because xylazine, an animal tranquilizer with no FDA-approved use in humans, is now pervasive in Philadelphia’s street fentanyl supply. Forensic testing has revealed xylazine’s presence in over 90% of street heroin and fentanyl samples, and Pennsylvania is considered the epicenter of the xylazine crisis.
Rachel McFadden is an emergency room nurse at the Hospital of the University of Pennsylvania and also works at a wound care clinic in Kensington in North Philadelphia that serves people who use drugs. She spoke with The Conversation U.S. about how to treat xylazine wounds and how the stigma around them prevents people from getting medical care and other help.
When did you start seeing xylazine wounds?
Before xylazine, most of the wounds we treated were skin infections like abscesses. These conditions develop when a bit of bacteria gets under the skin and a pocket of infection forms. When treated with antibiotics, these infections normally clear up quickly.
At the end of 2019, participants at the wound care clinic started to come in with a different kind of wound. They were filled with black and yellow dead tissue and tunneled deep into the skin. They were not wounds from infection but rather from tissue death or necrosis.
Initially, our clinic patients found that if they changed dope “stamps” – something like a brand in the unregulated drug market – the wounds would heal on their own. But by the end of 2020, people were developing these wounds no matter what stamp they used.
Even more troubling to me and the people I was seeing in the clinic was that the wounds seemed to develop on parts of the body where no injection had occurred, and even on patients who were snorting or smoking the dope and not injecting at all.

What causes the wounds?
The medical community does not fully understand what causes these wounds. Harm reduction advocates in Puerto Rico published the first reports on xylazine-associated wounds more than a decade ago, and research stemming from their experience found that the substance has direct cytotoxic effects. This means that when injected, xylazine will kill cells on contact and create pockets of necrosis under the skin.
Xylazine also constricts blood vessels, causes disease of the small vessels and lowers heart rate and blood pressure. Together, these effects restrict blood flow to the outermost reaches of our vascular system – namely, our skin and soft tissue. Tissue that is starved of oxygen and nutrients due to this restricted blood flow eventually become necrotic and slough away. So, exposure to xylazine via any route, not just injecting, can lead to small areas of tissue necrosis scattered across the body and prevent healing of other skin injuries like cuts and insect bites.
Not everyone in the scientific community is convinced there is a causal association between xylazine and these wounds. For example, I recently presented on a research panel during which another speaker suggested that a combination of fentanyl adulterants, or the ways in which people use, may be more to blame for the wounds.
In my opinion, this diversity of thought is good because it prompts more rigorous investigation into what’s really going on. But following the published literature and evidence as it has emerged, and working directly with people who use drugs, has convinced me of the connection.
How do you treat them?
There is a helpful wound care mnemonic – DIME – that I’ve adjusted slightly to summarize the most important aspects of treating these wounds. The D is for debridement, I is for infection and inflammation, M is for moisture management, and E is for environment.
Debridement: Debridement refers to getting rid of the dead or necrotic tissue, a hallmark of xylazine-associated wounds. Healing starts at the bottom or deepest part of the wound, but new tissue can’t form with layers of dead tissue blocking the way. In the clinic, we use ointments that gently and gradually dissolve the dead tissue. But a large buildup is best removed in the operating room, and we sometimes refer people to the hospital for this procedure.
Infection and inflammation: All sorts of bacteria proliferate on the dead tissue that accumulates in these wounds, forming what we call a biofilm. Bacterial biofilms embed in and around the necrotic tissue and form protective capsules, and they are unreachable by even intravenous antibiotics. They cause inflammation and can lead to infection, both of which stall wound healing. So we use strong antimicrobial ointments inside the wound that disrupt this biofilm, in addition to treating infections with antibiotics as they arise.
Moisture management: Our bodies are 70% water, and in areas without skin to hold all this fluid in – like these wounds – there is going to be a lot of drainage. In a xylazine-associated wound, the drainage picks up a foul odor from the necrotic tissue, and this is understandably highly distressing to people. Consequently, we often see people try to dry out their wounds in order to minimize the mess and odor. But wounds need moisture to heal, so we work with folks in the clinic to come up with a wound dressing that helps keep the wound bed moist while managing the drainage in a way that minimizes distress.
Environment: Living on the street with very limited access to showers, bathrooms or nutritious meals is a reality for many people using xylazine-adulterated fentanyl in Philadelphia. It is very difficult for people to keep up with a daily wound dressing change when even their most basic needs, including shelter, food and safety, are not met. I believe that advocating for resources and policies that address these basic needs is a critical piece of treating these wounds.
Providing high-quality wound care that also recognizes the lived experience and realities of people who use drugs is an art and a science. Last year, our nurse-led clinic published recommendations for xylazine-associated wound care based on our experiences providing this kind of care in Philadelphia. In January 2024, the Philadelphia Department of Public Health also released a comprehensive set of recommendations that I highly recommend for people wishing to learn more.

Where can people get treatment?
Few traditional health care settings in the area have set out to accommodate the needs of people with active substance use disorder who need wound care. For example, most outpatient wound care settings enforce strict scheduling and sobriety policies. Meanwhile, most hospitals supply inadequate pain and withdrawal management to patients with fentanyl and xylazine dependence, as evidenced by extremely high self-discharge rates in this population.
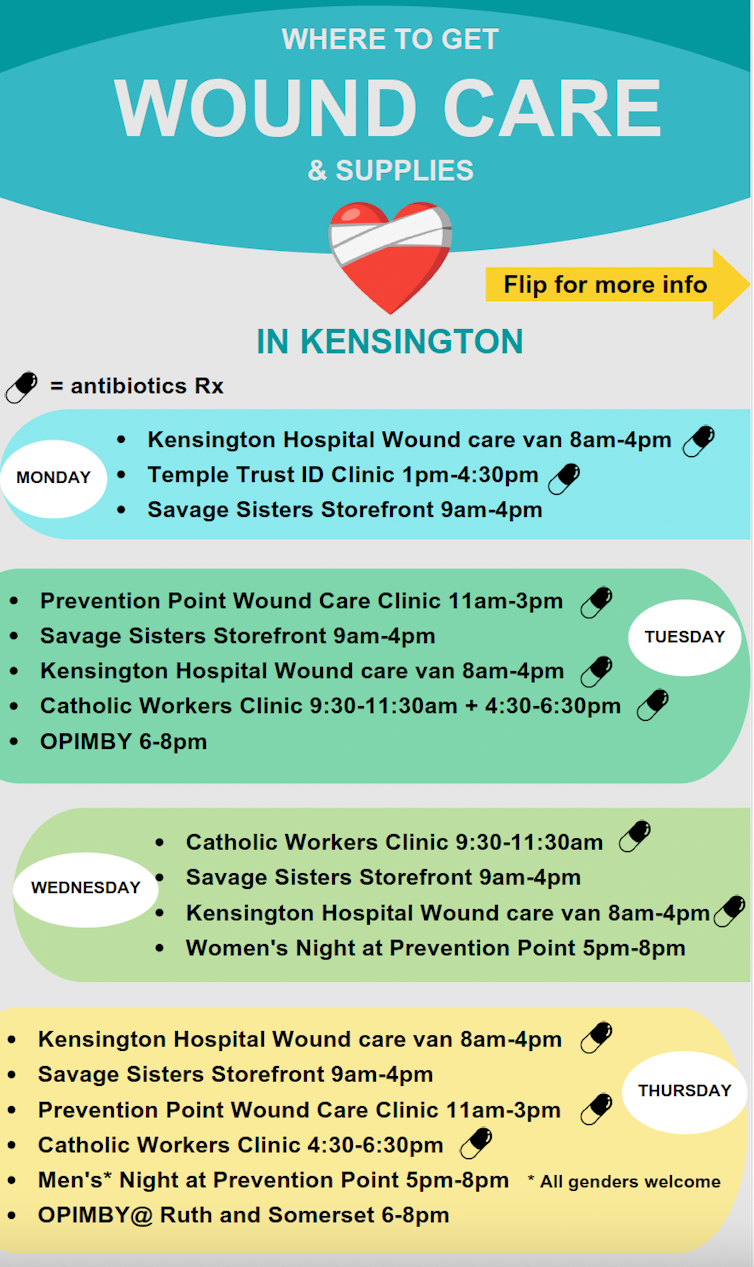
There are, however, a handful of low-barrier wound care clinics in Kensington, the North Philadelphia neighborhood at the epicenter of the xylazine epidemic. These walk-in settings don’t require insurance or payment and welcome people who are still using drugs. The city publishes a schedule of their locations and times.
But most of these clinics have limited hours, operate on shoestring budgets, rely on volunteers and donations, and are simply not equipped to offer the level of care that people often need.
How does stigma stop people from getting treated?
It is well documented that stigma around opioid addiction – perpetuated by health care workers and even by institutions and policies – can prevent people from getting the care they need.
For example, researchers at Thomas Jefferson University in Philadelphia found that people with xylazine-associated wounds are often denied admittance to detox and rehabilitation programs until their wound has healed. This is true even when they are medically stable and self-sufficient in their wound care.
On the flip side, patients who are receiving treatment for opioid use disorder and who require advanced medical care for their wounds are routinely rejected by skilled nursing facilities, which exist to support people with things such as wound care.
Our clinic patients have also reported experiencing humiliating treatment by staff at methadone clinics because of their wounds. And I have personally observed several instances in Philadelphia when an individual was denied a wound care intervention such as surgical debridement due to their drug use.
These barriers to treatment are highly unsettling, and I’ve sat with many clinic patients through emotional moments as they process the injustice of being denied care at every turn. I believe that providing support and encouragement to people who are suffering with these wounds, while holding health care settings and systems accountable, are equally important as we navigate this crisis.
I am a part-time nurse at Prevention Point Philadelphia, which is the location of the clinic that I mention in the article.
This article was originally published on The Conversation. Read the original article.







