Outpatients at St James’ Hospital feel better even before they see the doctor – thanks to a new note in hospital design. ‘Comfort while you wait’ is the new policy, and that means an informal atmosphere, extra comfy chairs, concealed lighting, heated cork floors, and an ultra-modern design throughout. No shades of depressing institutions here.
You might think this description comes from the glossy marketing material for one of today’s cutting-edge private hospitals. In fact, it’s from a 1954 Pathé News clip celebrating one of the earliest buildings designed for Britain’s fledgling National Health Service (NHS) – launched six years earlier on July 5, 1948.
What St James’ Hospital in Balham, south London, lacked in size, it made up for in ambition. The new central complex embodied the stated ideals of the NHS, to provide an equitable service for all citizens, free of charge and of the highest standard. The new buildings contained consulting rooms, staff offices and waiting rooms, and a children’s room that was lauded by the Pathé commentator:
In the children’s room, the longer the youngsters have to wait, the better they like it. They can play as loudly as they like, for in their own room their chatter and high spirits can’t worry other patients … It’s no wonder that in this hospital, some of the children and their parents come a little early for their appointments on purpose!
As we take stock of the NHS on the occasion of its 75th anniversary, most attention is focused on staff pay demands, lengthy waiting lists for treatment, and the intolerable pressures on staff during and beyond the pandemic. But the design and upkeep of NHS hospital buildings, and the impact these can have on the patients and staff who inhabit them, is another pressing, if less widely publicised, issue.

To mark the 75th anniversary of the launch of the NHS, we’ve commissioned a series of articles addressing the biggest challenges the service now faces. We want to understand not only what needs to change, but the knock-on effects on other parts of this extraordinarily complex health system.
I believe we can find answers to at least some of today’s health service problems by looking at the history of these buildings, and the shifting design priorities they reflect.
The story of St James’ Hospital is a case in point. Less than 40 years on from the proud launch of its new central complex, the entire hospital stood empty and ruinous – a symbol, perhaps, of the failed ambitions of the early NHS. The buildings were demolished in 1992, and the site was redeveloped for housing.

Parts of this hospital are sinking
Another south London hospital was in the news recently. “Patient safety at risk in crumbling hospital Boris Johnson promised to replace,” read a headline in the Observer, describing conditions in St Helier Hospital, Carshalton.

St Helier was built just before the outbreak of the second world war, constructed on reinforced concrete foundations with a steel-frame and brick infill, faced in white-painted cement render. At the time, it was regarded as the last word in up-to-date modernist design, with “accommodation of the highest class in any part of the world”.
Now, parts of this hospital are sinking. The basement floods, wards are sometimes forced to close, and the hospital has become “dilapidated and unpleasant”, according to Ruth Charlton, chief medical officer of Epsom & St Helier University Hospitals NHS Trust. In a recent commentary, she wrote:
Our ageing estate looked awful even when I joined, and over the years it’s decayed further before my eyes. Healthcare standards are getting higher while our hospitals are sliding into even more disrepair … Only last week we had to close one of our wards because the lift wasn’t working.
Nor is this an isolated case. In April, a tweet by palliative care doctor and author Rachel Clarke showed “an actual interior corridor of a major NHS hospital”. The photograph looks like the bowels of a particularly unsavoury multi-storey carpark, yet the reflection in the mirror clearly shows it is an internal space. The paint is peeling, the damp so bad that a streak of green algae is running down the corner of the room.
Along with such images of decay and dereliction, we have also seen images of egregious overcrowding over the past few years, as COVID-19 put extreme demands on NHS facilities that were already creaking badly. Accounts of patients being treated in corridors and even in hospital car parks continued last winter, even when the COVID threat had receded somewhat.
In January 2023, Alice Kenny, a junior sister at Queen’s Hospital in Romford, east London, who had been redesignated as a “corridor nurse”, told the BBC:
We don’t train to give care in corridors. It is really not nice and if we were in [our patients’] shoes, we’d be really upset as well. We’re supposed to look after patients like we do our own family, and we’re not able to do that.
The ideas and ideals of early NHS designs
As the architectural history of the NHS is such a huge subject, I have mainly focused on Scotland where I live and can access the official records – some of which have only become available to researchers in recent years. This has provided fresh insights into the ideas and ideals behind the design of the first purpose-built hospitals built by the NHS.
The problems back then were not dissimilar to those faced today: old worn-out buildings, staff shortages, rising costs and economic austerity. Take Old Monkland Home in Coatbridge, to the east of Glasgow – one of the 3,000-or-so hospitals that were transferred to state ownership when the NHS came into being in July 1948. A review of this former poorhouse’s facilities, published in a national hospital survey before the end of the second world war, was damning:
Old Monkland Home occupies a depressing site in Coatbridge. The hospital part now contains 69 beds, and there is also an asylum for milder types of lunatic … The impression is one of general neglect. The dining-room is very gloomy, the hospital is very little better than the main house, and the asylum block is totally unsuitable for patients of any kind. We are of the opinion that this institution is quite unsuitable for the care of the sick, and should be abandoned.
The NHS had inherited a patchwork of hospitals, predominantly over half-a-century old, that had been built to meet the medical needs of the time: sanatoria for tuberculosis, isolation hospitals for once-common infectious diseases such as measles and diphtheria, and cottage hospitals run by country GPs who carried out routine surgery, delivered local babies, set bones and treated wounds from accidents.

This article is part of Conversation Insights
The Insights team generates long-form journalism derived from interdisciplinary research. The team is working with academics from different backgrounds who have been engaged in projects aimed at tackling societal and scientific challenges.
There were also large urban workhouse infirmaries full of chronically ill elderly patients, huge mental hospitals, teaching hospitals, and convalescent homes. Funding to build and run them came from a wide range of sources, including public donations, church collections, the rates, government loans, and work-placed insurance schemes.
These buildings had been “built to last” 100 years or more (brick or stone buildings that were expensive to construct were only economically viable if they had a long lifespan). But they suffered from a lack of structural maintenance and redecoration during the war, and afterwards from the severe shortages of labour and materials.
The UK-wide survey of hospitals had been intended to inform post-war reconstruction and the development of a “national hospital service”, which aimed to “ensure that every patient requiring hospital treatment could obtain it without delay in the hospital most suited to their needs”. In reality, it painted a picture of uneven distribution and poor facilities, with the worst of the buildings being the old workhouses:
Wigtownshire Home, Stranraer, has not undergone any appreciable change since it was built about 1850. The building is worn out and dreary … This is a very poor place, and is quite unsuitable for housing the sick or aged, or indeed for any other purpose.
In the immediate post-war years, new housing was the most urgent requirement throughout Britain, along with new schools after the Butler Act of 1944 raised the school-leaving age to 15 (with a post-war baby boom to follow). Yet there was also a widespread consensus among the public that the current level of healthcare provision was no longer acceptable. A new type of hospital facility was needed to reflect the scientific advances of medicine and the aspirations of post-war Britain.
A five-star ‘hospital of the future’
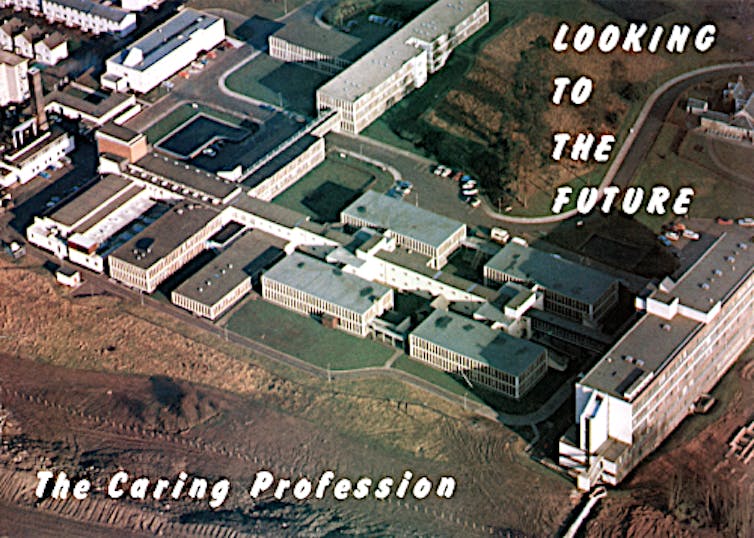
These aspirations found physical form in the first new general hospital built in Britain for the NHS, which opened in Scotland in 1955 at Vale of Leven to the north-west of Glasgow. One of its most striking features were the wards, which were dramatically different from the traditional “Nightingale-style” open wards that offered no privacy to patients.
At Vale of Leven, the beds were grouped in bays separated by glazed screens. Ceiling heights were lower to create a more homely feel. The day room was furnished like a domestic sitting room, with comfortably upholstered armchairs. Windows were set low enough in the walls for patients to be able to see the grounds while lying in bed – and they also provided natural ventilation, allowing fresh air and the sound of birdsong to enter each ward.
Facilities for staff were an important consideration, as the Architect & Building News explained:
A nurse’s station is an L-shaped counter containing knee space, drawers, filing cabinets etc, with a dwarf glass screen to cut off draughts, record board and shaded reading light, and small cupboards behind in the storage wall. The station is raised on a low step so that, when sitting, the nurse has a view of her 13 beds and, in fact, is only 25 feet away from her farthest patient and is quickly conscious of any movement or disturbance. Signal lights from beds are placed so that they can be seen from either of two nurse’s stations in case one is temporarily unoccupied.
The subject of hospital design was now a hot topic among architects, health professionals and administrators alike – with an emphasis on the collaborative planning processes and research-led design that had evolved in more progressive architecture schools before the war. Schools such as the Architectural Association in London and Liverpool had developed a belief in social theory and managerial efficiency. Architects sought specialist advice on every aspect of the hospital, from the wards to catering and even laundries. As the regional architect for the South Eastern Regional Hospital Board wrote in 1951 about his new building schemes:
It would be futile for medical science to progress and leave in its wake a dull, unimaginative architecture.
Another reason for the extra care being taken over these new buildings was that, in the period of full employment in the 1950s and ‘60s, it was often proving difficult to attract enough hospital staff. The shortage of nurses, traditionally a female role, was especially acute because the rate of pay was lower than for many office jobs in the private sector – jobs that also offered shorter hours and fewer pressures than nursing.
To entice new recruits and enhance retainment levels, local management boards pushed hard to get well-appointed nurses’ homes built and to provide generous staff social and recreational facilities – from tennis courts to swimming pools, coffee bars to halls for cinema shows and dances.
At this time, the opening of a new hospital was a newsworthy event, featured in the architectural and medical press, national and local newspapers, and in newsreels. The opening of the new High Wycombe General Hospital in the mid-1960s was met with another gushing tribute from the Pathé News team:
The spaciousness of the entrance and reception hall will give patients confidence that here they are meeting medical science 1967-style, equipped as it should be. Gone is the old atmosphere of healing on the cheap, gone too is the belief that staff of the hospitals should put up with third-rate food and bad quarters. The menus in the nurses’ dining room are varied and make eating a pleasure deserved by women whose devoted service goes far beyond the minimum they could get away with.
I remember this hospital (more commonly known as Wycombe General) from not long after the film was released. It was where I had a tonsillectomy – then a routine operation – at the age of seven. I recall the hospital being shiny and modern, with toilets that were spotlessly clean and, unlike our loo at home, heated!
I remember the children’s ward being a bright sunny room with about eight beds, and a small dayroom where we had breakfast that was made rather cramped by an enormous toy cupboard, where a kind nurse hid my bowl of porridge which I could not eat. I had no trouble with the ice cream we were allowed to have in bed after our operations, though.
Our parents only visited for a short time during the day, but we didn’t seem to mind or feel anxious about it – perhaps in part because of the atmosphere in the hospital, where modern architecture conveyed, even to a young child, confidence in medical science. As the Pathé commentator concluded:
There is a good reason for High Wycombe General being called a five-star luxury hospital. It’s part of the new approach to the art and science of getting sick people well.
Fast-forward just over half a century, however, and Wycombe General is now “approaching its end of life” and in “dire need of replacement”, according to the NHS trust that runs it. While confirming to the BBC that the hospital is still “safe”, the hospital’s ongoing repairs and maintenance now cost the trust around £2 million a year.

The ambitious plan quickly comes off the rails
Wycombe General was built following a period when funding for hospital building had increased by over 50%. In 1962, the UK government had published its Hospital Plan, which promised that 90 new hospitals would be commenced in England and Wales by 1971. The plan was to provide a network of new district general hospitals evenly distributed around the country, so that everyone would be in easy reach of all the main hospital services, with just a few of the more unusual specialities based at a regional centre.
However, it did not take long for this ambitious plan to come off the rails. Not enough money had been pledged by the government to fund all the schemes that were proposed, the process of planning and design took a long time, costs escalated, and by 1964, comprehensive revisions had to be made. In successive years, the plans were scaled back.
By the mid-1960s, relatively little had been achieved and the policy of concentrating on district general hospitals was questioned. The 1966 revision of the Hospital Plan refocused the building programme towards creating units for the elderly and mentally ill. Start dates for new hospitals were postponed and, to try to combat rising costs, stricter financial controls were introduced.
Despite this, there was still a belief in producing good quality buildings designed to meet the needs of modern medicine in attractive surroundings. As the Architects’ Journal put it when discussing the new staff restaurant and stores building at Kingston Hospital in Surrey:
The matter of nurses’ meals is almost a household topic and, along with spectacles and false teeth, has been giving the health ministry a bad press.
At Falkirk Royal Infirmary in Scotland’s central belt, meanwhile, an experimental surgical ward unit was designed around new ways of organising nursing on the lines of progressive patient care, while also making the nurses’ routines easier and reducing the amount of walking they would have to do. Hospital infection and resistance to antibiotics were already a concern in the 1960s, and engineers designed more sophisticated heating and ventilation systems to control the movement of airborne infections and prevent cross infection.
Unfortunately, such considerations cost more than the government was willing to spend, and no health minister of either political persuasion was able to convince the cabinet or the Treasury to provide the amount of money that the rebuilding programme was going to cost.
The 1970s was a period of devaluation of sterling, strikes and war in the Middle East that caused an oil crisis. There was a three-day week, petrol rationing and power cuts. This led to public spending cuts that only worsened the position for the hospital building programme. At the same time, there was widespread criticism of the amount of time it was taking to build each hospital, and concern that a number of recently completed hospitals had been found to have structural defects.

A case in point is the saga of Inverclyde Royal Hospital in Greenock, west Scotland – one of the new district general hospitals promised in the original Hospital Plan. After a provisional cost limit of just over £4 million was approved in 1964, a design team was appointed the following year. However, the UK government halted the project for nearly two years due to a shortage of funds – a time when lots of large national projects were being halted. At the same time, the design brief had to be revised to keep up-to-date with technical guidance.
Amid new tenders, spiralling budgets and a further cost reduction exercise, work finally started on site in 1970, but the official contract completion date of March 1976 was missed, and the fabric of the building was eventually completed in November 1977 – only for the ventilation systems to be found to be defective.
It was not until the very end of 1979 that Inverclyde Royal Hospital was finally completed, at a cost of over £13m – more than three times the original cost limit. There was no single reason for the vastly increased cost, but the era’s high inflation rates were a significant factor. Each delay led to the cost going up, cancelling out the cost reduction exercise. Time and again on new hospital schemes, such exercise led to the use of poorer-quality materials and inferior heating and ventilation systems, which would cause problems with the building later on.
But more fundamentally, the new hospitals being built were now anticipated to last only between 40 and 50 years at the most. The reasons why this changed from the Victorian era when hospitals were built to last for a century or more, are many and complex. The main reason was the increasingly rapid advances being made in medical science, which led to a widespread view that the buildings would become obsolete as medical needs evolved.
But 40 is no age to be consigned to the scrap heap. We do not expect our homes to expire after such a short timespan – but equally, we understand that we need to invest in maintenance to keep them in good condition.
As the NHS celebrates its 75th anniversary, many of its hospitals built in the 1960s, ‘70s and early ‘80s have reached the end of their anticipated lifespan. As a result, the UK is now having to tackle the problem of large numbers of hospitals that have reached the end of their predicted lives.
Part of Johnson’s 2019 general election manifesto promised that 40 new hospitals would be built by 2030. There was talk of “levelling up our NHS” and a determination “to build back better”. However, this plan was later exposed as something of a numbers trick or “mirage”, with many of the “new” hospitals turning out to be extensions or refurbishments. In February 2023, the Observer reported that only ten of the projects had secured full planning permission, with one NHS trust leader warning that: “Some hospitals are literally falling down.”
Downgrading ambitions from ‘ideal’ to ‘adequate’
Search for King’s Lynn’s Queen Elizabeth Hospital online, and you are likely to find multiple news items about its dilapidated condition, demands to hasten its replacement, and images of ceilings being held up by acrow props.
“Isn’t it lovely,” the Duchess of Kent had told the Lynn Advertiser when she first entered the new hospital in July 1980. According to the same newspaper, the public had been similarly impressed when given guided tours of the newly completed building:
Guides pointed out bright wards … most with outlooks over landscaped gardens. Mouths dropped as guides said patients would be able to choose the main course of their meals from a menu offering 17 options – and every three weeks, that menu would be changed.
Yet, just 43 years later, the Queen Elizabeth has been described as “Britain’s most dilapidated hospital”. According to a report on the Norfolk Live website:
Patients lie in bed looking up at the [roof] supports … Regular checks take place every day to make sure the roof is not at more risk of collapse through holes in the concrete described as being ‘like an Aero chocolate bar’.
The Aero bar analogy refers to the reinforced, autoclaved aerated concrete (RAAC) used in the hospital roof’s construction, and in many other public buildings. In 2018, the roof of a primary school in Kent collapsed only a day after “signs of structural stress” had appeared in the staffroom ceiling. It transpired that the roof had been constructed of RAAC, which has an estimated shelf-life of just 30 years.
An initial investigation into the use of RAAC in schools has recently been extended to look at public buildings more widely – including hospitals. In May, a report on the Conservative government’s promise to build 40 new hospitals suggested that just five – those that had used RAAC in their construction – were now being prioritised.
The Queen Elizabeth was one of the so-called “best buy” hospitals designed by the Department of Health & Social Security (DHSS) as a complete package. These were introduced in 1967 to remedy the problems of drawn-out design processes and escalating costs that had been derailing the NHS hospital building programme. It was a budget version of the district general hospital envisaged in the 1962 Hospital Plan, providing fewer beds per head of population in more confined spaces using simpler construction methods.
Standardisation and prefabrication were the principles of this design process, which was intended to provide an “adequate” rather than “ideal” hospital amid the country’s deep financial challenges of the 1970s. Hospital design was pared back to its essentials – a policy that has largely continued ever since.
The “nucleus” hospitals that followed from the mid-1970s were designed to limit new developments and major extensions to a nucleus of departments costing no more than £6 million (at 1975 prices). Every possible means of economising space and services was explored by the Hospital Building Division within the DHSS.
Crucially, a lower complement of beds per hospital was provided, based on the justification that earlier patient discharges would create a more intensive use of diagnostic and treatment facilities. In other words, Britain’s hospitals were now becoming high-turnover factory lines.

Good design can be life-enhancing
As hospitals at the end of their lifespan struggle to deal with patient overcrowding amid crumbling facilities, have decades of cost-cutting exercises when it comes to hospital design and construction turned out to be a false economy? Can a price be put on the damaging effects of poor hospital design on staff morale or patient health?
While we can put a figure on the cost of buying in agency staff to cover staff shortages or even major building repairs, less quantifiable is the impact on health and wellbeing of the buildings themselves.
But we know that good design can be life-enhancing. Within the NHS, Maggie’s centres are a network of cancer drop-in centres unified by a groundbreaking commitment to pushing architectural boundaries, with their multi-award-winning buildings having been designed by some of the world’s leading architects such as Frank Gehry and Zaha Hadid.
These centres, located throughout the UK and also in Hong Kong, offer “unique physical environments” created on the basis of a wide body of evidence that shows how aspects of physical space affect us.
The impact of design on inpatient wellbeing has been a growing focus of research for many years, highlighting the importance of obvious elements such as access to nature, attractive surroundings, artworks on walls, single rooms for patients. There is, for example, evidence for the therapeutic benefits of “healing gardens”, and gardening or outdoor exercise is sometimes prescribed by GPs.
More recently, consideration of therapeutic spaces has broadened to include hospital staff as well as patients, in order to tackle the high levels of sickness absence, distress and burnout among healthcare professionals – levels that are higher in this sector than any other. Yet most solutions so far offered have been short-term interventions, rather than a fundamental reassessment of how the workplace should be designed with staff wellbeing placed on the same footing as patient wellbeing.
Designing a hospital in which it is a pleasure both to work and be a patient is surely a goal worth achieving, and one which it is possible to justify on economic grounds. Spending more now on hospital buildings can save having to rebuild, at higher costs, in 20 or 30 years’ time. If done in such a way as to attract new staff, it can reduce the amount spent on agency fees.
Good design does not have to mean a new hospital, even if that is what people believe they want. Promising to build new hospitals is good publicity for any government, but it can also lead to damning headlines about wildly increased costs and failed promises further down the line.
Good design can also be achieved through retrofitting, by altering and adapting existing buildings. It is a more sustainable route and ideally would be the first option considered in the face of the present climate emergency. It is a complex issue, and retrofitting may be impossible in some cases – and very probably more expensive than a new-build in almost every other case. However, it addresses the issues of the embodied carbon in existing buildings.
Political pressures to win public votes favours the quick fix. We need a new way of thinking about building, adapting and retrofitting hospitals that can deliver comfortable environments in a sustainable way for the long term, and to understand that cost-cutting today often leads to greater expense in the future.
In 2021, the Wolfson Economics Prize set as its challenge the planning and design of the hospital of the future, specifically with a view to “radically” improving patient experiences, clinical outcomes, staff wellbeing and integration with wider health and social care.
The designers of British hospitals in the 1950s and ‘60s – in the early years after the launch of the bold new NHS – might be surprised to find we are still asking the same questions they set out to solve all those years ago.

For you: more from our Insights series:
To hear about new Insights articles, join the hundreds of thousands of people who value The Conversation’s evidence-based news. Subscribe to our newsletter.
Harriet Richardson Blakeman receives funding from AHRC for doctoral research.
This article was originally published on The Conversation. Read the original article.