
What’s the difference? is a new editorial product that explains the similarities and differences between commonly confused health and medical terms, and why they matter.
Changes in thinking and memory as we age can occur for a variety of reasons. These changes are not always cause for concern. But when they begin to disrupt daily life, it could indicate the first signs of dementia.
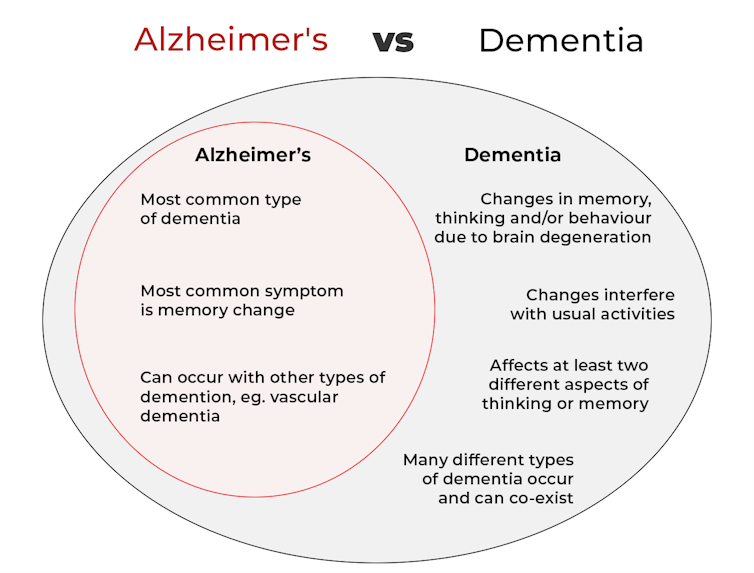
Another term that can crop up when we’re talking about dementia is Alzheimer’s disease, or Alzheimer’s for short.
So what’s the difference?
What is dementia?
Dementia is an umbrella term used to describe a range of syndromes that result in changes in memory, thinking and/or behaviour due to degeneration in the brain.
To meet the criteria for dementia these changes must be sufficiently pronounced to interfere with usual activities and are present in at least two different aspects of thinking or memory.
For example, someone might have trouble remembering to pay bills and become lost in previously familiar areas.
It’s less-well known that dementia can also occur in children. This is due to progressive brain damage associated with more than 100 rare genetic disorders. This can result in similar cognitive changes as we see in adults.
So what’s Alzheimer’s then?
Alzheimer’s is the most common type of dementia, accounting for about 60-80% of cases.
So it’s not surprising many people use the terms dementia and Alzheimer’s interchangeably.
Changes in memory are the most common sign of Alzheimer’s and it’s what the public most often associates with it. For instance, someone with Alzheimer’s may have trouble recalling recent events or keeping track of what day or month it is.

We still don’t know exactly what causes Alzheimer’s. However, we do know it is associated with a build-up in the brain of two types of protein called amyloid-β and tau.
While we all have some amyloid-β, when too much builds up in the brain it clumps together, forming plaques in the spaces between cells. These plaques cause damage (inflammation) to surrounding brain cells and leads to disruption in tau. Tau forms part of the structure of brain cells but in Alzheimer’s tau proteins become “tangled”. This is toxic to the cells, causing them to die. A feedback loop is then thought to occur, triggering production of more amyloid-β and more abnormal tau, perpetuating damage to brain cells.
Alzheimer’s can also occur with other forms of dementia, such as vascular dementia. This combination is the most common example of a mixed dementia.
Vascular dementia
The second most common type of dementia is vascular dementia. This results from disrupted blood flow to the brain.
Because the changes in blood flow can occur throughout the brain, signs of vascular dementia can be more varied than the memory changes typically seen in Alzheimer’s.
For example, vascular dementia may present as general confusion, slowed thinking, or difficulty organising thoughts and actions.
Your risk of vascular dementia is greater if you have heart disease or high blood pressure.
Frontotemporal dementia
Some people may not realise that dementia can also affect behaviour and/or language. We see this in different forms of frontotemporal dementia.
The behavioural variant of frontotemporal dementia is the second most common form (after Alzheimer’s disease) of younger onset dementia (dementia in people under 65).
People living with this may have difficulties in interpreting and appropriately responding to social situations. For example, they may make uncharacteristically rude or offensive comments or invade people’s personal space.
Semantic dementia is also a type of frontotemporal dementia and results in difficulty with understanding the meaning of words and naming everyday objects.
Dementia with Lewy bodies
Dementia with Lewy bodies results from dysregulation of a different type of protein known as α-synuclein. We often see this in people with Parkinson’s disease.
So people with this type of dementia may have altered movement, such as a stooped posture, shuffling walk, and changes in handwriting. Other symptoms include changes in alertness, visual hallucinations and significant disruption to sleep.
Do I have dementia and if so, which type?
If you or someone close to you is concerned, the first thing to do is to speak to your GP. They will likely ask you some questions about your medical history and what changes you have noticed.
Sometimes it might not be clear if you have dementia when you first speak to your doctor. They may suggest you watch for changes or they may refer you to a specialist for further tests.
There is no single test to clearly show if you have dementia, or the type of dementia. A diagnosis comes after multiple tests, including brain scans, tests of memory and thinking, and consideration of how these changes impact your daily life.
Not knowing what is happening can be a challenging time so it is important to speak to someone about how you are feeling or to reach out to support services.
Dementia is diverse
As well as the different forms of dementia, everyone experiences dementia in different ways. For example, the speed dementia progresses varies a lot from person to person. Some people will continue to live well with dementia for some time while others may decline more quickly.
There is still significant stigma surrounding dementia. So by learning more about the various types of dementia and understanding differences in how dementia progresses we can all do our part to create a more dementia-friendly community.
The National Dementia Helpline (1800 100 500) provides information and support for people living with dementia and their carers. To learn more about dementia, you can take this free online course.
Nikki-Anne Wilson does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
This article was originally published on The Conversation. Read the original article.







