If a drug could be said to be having a blockbuster moment, then 2023 is as much Ozempic's year as it is Pedro Pascal's.
Since the diabetes drug caught on among celebrities looking to shed a few pounds before awards season, inventory has been flying off pharmacy shelves. Prescriptions reached a high in late February, and reports of shortages throughout the U.S. abounded, profoundly affecting the people with diabetes who take the drug for that chronic condition. With the hype came the money: Behemoth weight loss company Weight Watchers acquired telehealth service Sequence, which offers Ozempic prescriptions, in April.
Ozempic does seem to cause reliable weight loss, though it’s far from dramatic. One 40-week study found that over the course of about 10 months, participants on 1 milligram of Ozempic lost up to 13 pounds while those on 2 milligrams lost about 15 pounds.
But alongside this weight loss are side effects, like the inability to concentrate, nausea, GI troubles, muscle loss, and reports of weakened bones. Anecdotally on social media, Ozempic users trade stories about neurological side effects, some documented and some not, like brain fog and sleeplessness. Some even report bizarre dreams, like Clint Eastwood assisting them at Home Depot or shoe shopping with Jeff Goldblum.
“Once you talk about brain circuitry, you have these really complex circuits that send off collaterals projecting to other parts of the brain...They can have secondary effects on cognition and so forth.”
That nausea might be a side effect of a drug that hijacks how you eat and process food may not be a surprise. But the brain fog speaks to a bigger, much murkier issue: Neuroscientists don't fully understand how Ozempic and drugs like it affect the brain long-term, especially for people taking the prescription for something it wasn’t originally intended for.
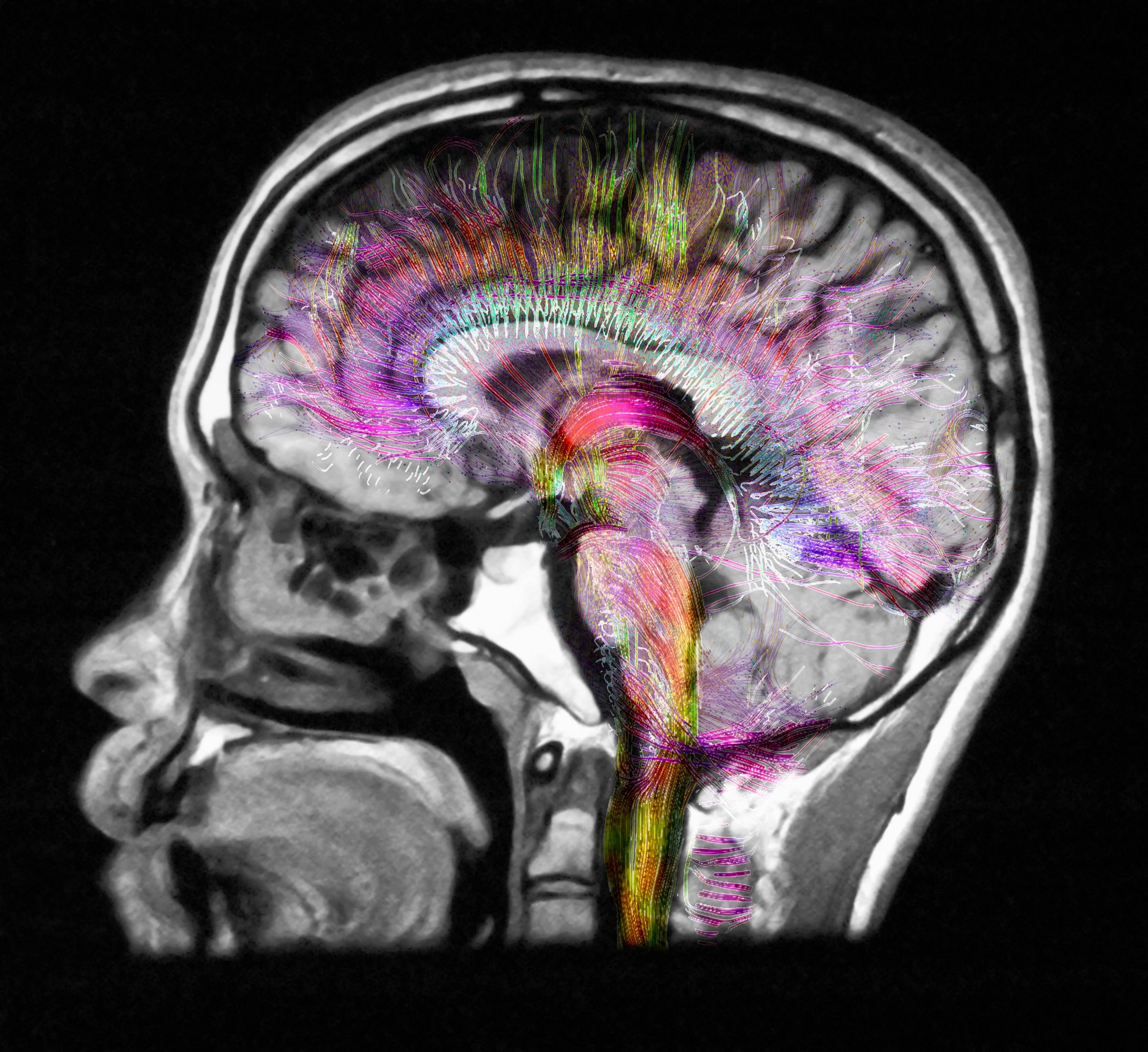
“Once you talk about brain circuitry, you have these really complex circuits that send off collaterals projecting to other parts of the brain,” Zachary Freyberg, an associate professor of psychiatry and cell biology at the University of Pittsburgh School of Medicine, tells Inverse. “They can have secondary effects on cognition and so forth.”
The crux of Ozempic is that it seems to dull the activity in the hunger centers of the brain, which in turn makes you eat less and experience fewer cravings. But one of the challenges of neuroscience is that while we know a lot about the brain, there’s a lot more we don’t know. This extends to the neuroscience of obesity and the circuits involved in controlling hunger and eating behaviors. Inverse spoke to several experts studying Ozempic and drugs like it to try and understand how much we know, and don’t know, about how these drugs influence our brain’s delicate chemistry.
Ozempic and the brain
The active ingredient in Ozempic and Wegovy is semaglutide, which belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists. These are used to treat type two diabetes.
Typically after you eat a meal, cells in the intestine release GLP-1 and the signal travels up to the brain to bind to specific receptors located in an area called the hypothalamus, particularly the arcuate nucleus involved in regulating hunger and satiety signals, Priya Jaisinghani, an endocrinologist and obesity medicine specialist at New York University Langone Medical Center, tells Inverse.
In the arcuate nucleus, two neurons — the cocaine- and amphetamine-regulated transcript (or CART) and proopiomelanocortin (POMC) — pump up their activity, helping you feel full. Other neurons that make a protein called neuropeptide Y are told to stand down, decreasing feelings of hunger.
But these effects aren’t confined to the brain. GLP-1 (or semaglutide) can slow the rate at which your stomach empties, leading to a longer-lasting feeling of fullness. It can also decrease the production of the hunger hormone ghrelin, which further reduces appetite.
But this pathway is only one of three pathways our brains use to regulate appetite, David Lau, professor emeritus of medicine, biochemistry, and molecular biology at the University of Calgary, tells Inverse.
“We still don’t know quite exactly how that works.”
The other two are the hedonistic pathway associated with reward and pleasure aspects of eating — like craving ramen in the middle of the night — and the cognitive or executive pathway that involves higher-order brain regions like the prefrontal cortex.
“What’s interesting to notice [is that] GLP-1 receptor agonists also affect cravings, which means they have some effect on the hedonistic pathway,” says Lau. “We still don’t know quite exactly how that works.”
What we still don’t understand about Ozempic and the brain
Our understanding of how Ozempic is involved in appetite regulation is mostly based on animal studies.
But animal models are only proxies — they can’t fully resolve what’s going on in the human body. Lau acknowledges there may be hidden aspects of appetite wiring or GLP-1 receptor neurogeography we’re not entirely sure of since doing those investigations in humans can be challenging, technologically and ethically speaking.
Not to mention, neurons like CART neurons aren’t only located in the arcuate nucleus of the hypothalamus. Among many places, they dot the nucleus accumbens, a small structure located deep within the brain in the basal ganglia. It's part of a larger brain system known as the reward pathway or the mesolimbic pathway that’s been associated with addiction and drug abuse. Curiously, this tracks with another of the anecdotal side effects users report is that their desire to drink alcohol disappears with Ozempic, although that is not well studied.
This brings us to this crucial question: Does Ozempic and its kin only affect the parts of the brain we know are involved in appetite regulation? Do we know the full extent to which these drugs influence the brain's neurochemistry?
At present, Freyberg says, the answer is a definitive no.
But because Ozempic does act on the brain, it is likely it has some secondary effects. This could explain why some Ozempic and Wegovy users have brain fog or entertain vivid, star studded dreams. As for the latter, a Novo Nordisk spokeswoman told the Wall Street Journal in April the company didn’t have enough information to establish whether the drugs were causing the dreams.
“This is not the first time we’ve heard of this,” says Jaisinghani. “There are other drugs that can cause very vivid dreams.” Such medications include antidepressants, stimulants like Ritalin, and the smoking cessation drug Chantix.
“I would never say GLP-1 receptor agonists don’t cause brain fog because this could potentially be a downstream effect among very few people. Rare, but it could be a real occurrence,” says Lau. “[But] we need to be very skeptical and careful of what patients report, and we need to make sure that this is not just an association but truly an effect of the medication. The only way to do that is by having post-marketing surveillance.”
Jaisinghani, Lau, and Freyberg say with time, it’s likely we’ll learn more about the brain in terms of mapping GLP-1 receptors and whether these buzzy weight loss injectables indeed cause any neural side effects unrelated to appetite control. Semaglutide is being considered as a potential treatment for Alzheimer’s and Parkison’s disease, and other clinical trials are looking at how the drug could help individuals with polycystic ovarian syndrome.
If you are interested in taking Ozempic, then the great unknowns about how it affects the mind and body mean it is critical that you see a specialist before hopping on the hype train.
“Weight loss is not a one size fits all,” says Jaisinghani. “You want to make sure you’re really [getting] into the underlying root cause of what may be contributing to a disease like living with obesity and have the adequate physical evaluation or assessment… [otherwise] the real cause may not be addressed.”
Ultimately, what weight loss does to the body and brain is far more delicate and nuanced than the simple flip of numbers on a scale.







