In the majority of cases, children who catch COVID won’t end up suffering serious illness. Kids have fewer symptoms, less severe disease, and tend to recover faster than adults.
The best case scenario for children sees them having relatively manageable symptoms, recovering fully, and soon testing negative. As researchers, we wanted to understand why some children have a far worse experience.
If they don’t recover, children with COVID can go on develop two different disorders. The first is Multisystem Inflammatory Syndrome in Children (MIS-C) where patients have painful inflammation on their skin, eyes and even internal organs such as the heart, lungs, and brain. The most fascinating (and confusing) thing about MIS-C is it never occurs in adults, only children. The second disorder is Acute Respiratory Distress Syndrome (ARDS), a life-threatening respiratory failure as a result of serious COVID.
By comparing blood samples from healthy children and those with serious COVID, we identified two sets of proteins that were switched on in kids with these frightening syndromes.
Read more: Multisystem inflammatory syndrome after COVID in children is rare but makes the body fight itself
Searching for the triggers
We have spent the past two years trying to understand how children’s bodies deal with COVID, and why it is so different from adults. Through our research, we wanted to understand exactly what the virus does to children to trigger a small number of them to develop MIS-C or ARDS, so we could help to figure out new ways of diagnosing or even treating them.
You may have heard of genomics – a scientific technique that can investigate all of a person’s genetic information (their genome) at once. In our study, we used proteomics which allows us to look at hundreds of proteins (the proteome) simultaneously.
Whenever something changes in the body (such as catching a virus like COVID) it can cause changes to your proteome. This helps tell us which systems of the body are affected.
We took blood samples from healthy children (collected at the Royal Children’s Hospital, Melbourne) and compared them to blood samples from children with MIS-C or ARDS (collected at the Hôpital Necker Enfants Malades, France). We performed proteomic experiments on the samples and found hundreds of proteins from each patient.
When we compared the amount of each protein in samples from children with severe COVID to the healthy blood samples, we found there were 85 proteins that changed in MIS-C and 52 proteins that changed in ARDS.
Read more: Got a child with COVID at home? Here's how to look after them
Blood clotting and immunity play a role
Listing a set of proteins is just the first step. It’s really important for us to know exactly what functions these proteins have in the body. By understanding the role each of those proteins plays, we can start to understand the biology underneath the disease.
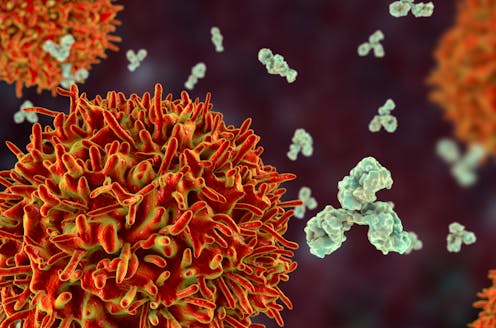
Proteins that control blood-clotting and the immune system were affected in both MIS-C and ARDS patients, telling us these systems play an important role in severe COVID. We were also able to show that children with MIS-C have affected proteins connected to B cells (which help facilitate an immune response) and antibodies (which fight off foreign invaders in the body). Meanwhile, children with ARDS have affected proteins connected to the breakdown of red blood cells (which transport oxygen around the body).

Read more: Do kids get long COVID? And how often? A paediatrician looks at the data
Our work continues
Fortunately, cases of MIS-C and ARDS are rare. But that doesn’t mean we shouldn’t try to understand how they work. Especially when severe COVID is so dangerous for the children affected and frightening for their families.
By narrowing down the potential blood proteins involved in severe COVID from hundreds down to less than 100, we can hone in on developing better diagnostic and treatment information.
This study was part of our larger research aim, which was to understand how COVID impacts adults and children differently.
We’ve already been able to show that platelets (small blood cells that trigger clotting) activate in adults and children, while blood clots formed in children due to COVID are more porous and less stable.
The author wishes to acknowledge the strong collaborations between the University of Melbourne, the Royal Children’s Hospital, the Royal Children’s Hospital Foundation, Murdoch Children’s Research Institute, Hôpital Necker and the Australian Proteome Analysis Facility that made this work possible.
Conor McCafferty does not work for, consult, own shares in or receive funding from any company or organization that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
This article was originally published on The Conversation. Read the original article.



.png?w=600)



