Mental illnesses such as obsessive compulsive disorder, depression and addiction are notoriously hard to treat and often don’t respond to drugs. But a new wave of treatments that stimulate the brain with electricity are showing promise on patients and in clinical trials. In this episode of The Conversation Weekly podcast, we talk to three experts and one patient about the history of treating mental illness, how new technology and deeper understanding of the brain are leading to better treatments and where the neuroscience of mental illness is headed next.
It’s not uncommon to hear people joke about how their “OCD” makes them want to straighten a crooked picture or clean a smudge on a countertop, but for people actually living with severe obsessive compulsive disorder, the reality is anything but funny.
Moksha Patel is a physician and professor at the University of Colorado and has severe OCD. “OCD was really taking over my life. The most obvious of my symptoms were not being able to use any public restrooms, showering for an hour after using the restrooms each time and using chemical cleaners on my skin and my mouth,” he says. After struggling for years, Patel eventually connected with Rachel Davis, a psychiatrist and researcher also at the University of Colorado. Davis suggested that he could be a good candidate for deep brain stimulation as a treatment for his OCD.
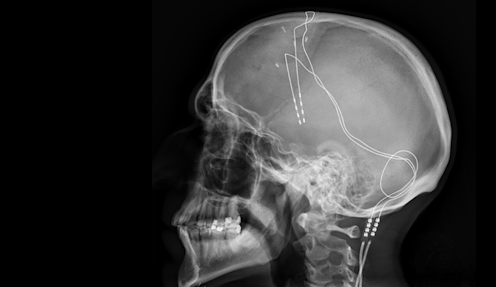
“Deep brain stimulation involves the implantation of electrodes in the deeper areas of the brain,” Davis explains. These electrodes then transfer into the brain itself small electrical currents that a doctor and their patient try to tune correctly. As Davis explains, “Basically we’re looking to find the settings where the patient feels that their mood is better, their anxiety is less and they have more energy.”
Deep brain stimulation works well for a lot of patients and has only started to get mainstream attention in the past decade or so, but ideas underlying this treatment are nearly 60 years old. As explained by Joseph Fins, a neuroethicist and professor of medicine at Wei Cornell Medical College, part of Cornell University in the US, it all started with a Spanish neuroscientist named Jose Manuel Rodriguez Delgado in 1964. “He put a thing called the stimoceiver, a deep brain stimulator, into the brain of a charging bull. And with an electrical current controlled by radio frequency, he was stop the bull in its tracks.”
While this work got Delgado on the front page of The New York Times, it came on the heels of a horrific era of mental health treatment that involved lobotomies, electroshock therapy and many other destructive and deeply unethical interventions. So when researchers began to discover drugs that could help people with mental illness, Fins says “psychosurgery and these types of somatic therapies began to fall out of favor and physicians moved away from more physical interventions.”
As modern neuroscience led to better understanding of how the brain works, and stigma surrounding physical treatments faded, deep brain stimulation got its second chance in the sun. And as technology has improved, researchers like Jacinta O'Shea, a neuroscientist at the University of Oxford have begun to study a noninvasive technique for stimulating the brain with electricity, called transcranial magnetic stimulation.
“If you place a ferromagnetic coil on the scalp and pass a rapidly changing electrical current through that coil, it will induce an electric field that passes painlessly through the skull and into the brain tissue underneath,” O'Shea explains. And just as with deep brain stimulation, these electrical fields can help people overcome mental health issues like depression.
Researchers still don’t quite know how deep brain stimulation or transcranial magnetic stimulation work, but with every new treatment, they are learning more about the complicated world of the brain and taking steps toward the treatments of tomorrow.
Listen to the full episode of The Conversation Weekly to find out more.
This episode was produced and written by Katie Flood and Daniel Merino, with sound design by Eloise Stevens. The executive producer was Gemma Ware. Our theme music is by Neeta Sarl.
You can find us on Twitter @TC_Audio, on Instagram at theconversationdotcom or via email. You can also sign up to The Conversation’s free daily email here. A transcript of this episode will be available soon.
Listen to The Conversation Weekly via any of the apps listed above, download it directly via our RSS feed, or find out how else to listen here.
Jacinta O'Shea has consulted for Welcony Inc and is currently on the Scientific Advisory Board of Plato Science. She receives research funding from the Wellcome Trust/Royal Society and the Academy of Medical Sciences in the U.K. Joseph Fins receives funding from the U.S. National Institutes of Health BRAIN Initiative, Dana Foundation, Greenwall Foundation, Robert Wood Johnson Foundation, Buster Foundation, NIH CTSC, NIH Eunice Kennedy Shriver National Institute of Child Health, Blythedale Children’s Hospital and from numerous editorial boards. He is also the president of the International Neuroethics Society, Chair-Elect and board member of The Hastings Center and a Trustee Emeritus at Wesleyan University. Trustee Emeritus, Wesleyan University.
Rachel Davis consults for Medtronic, Inc. She receives funding from the U.S. National Institutes of Health. Moksha Patel has nothing to disclose.
This article was originally published on The Conversation. Read the original article.







