Ticks are the wiliest of blood feeders. With a single bite, they inject a potent payload of saliva filled with enzymes that prevent your body from feeling pain. These tactics allow the tick to feed for days undetected. However, lurking within this teeny glob of spit is something far more sinister: Borrelia burgdorferi, the invasive bacteria behind Lyme disease.
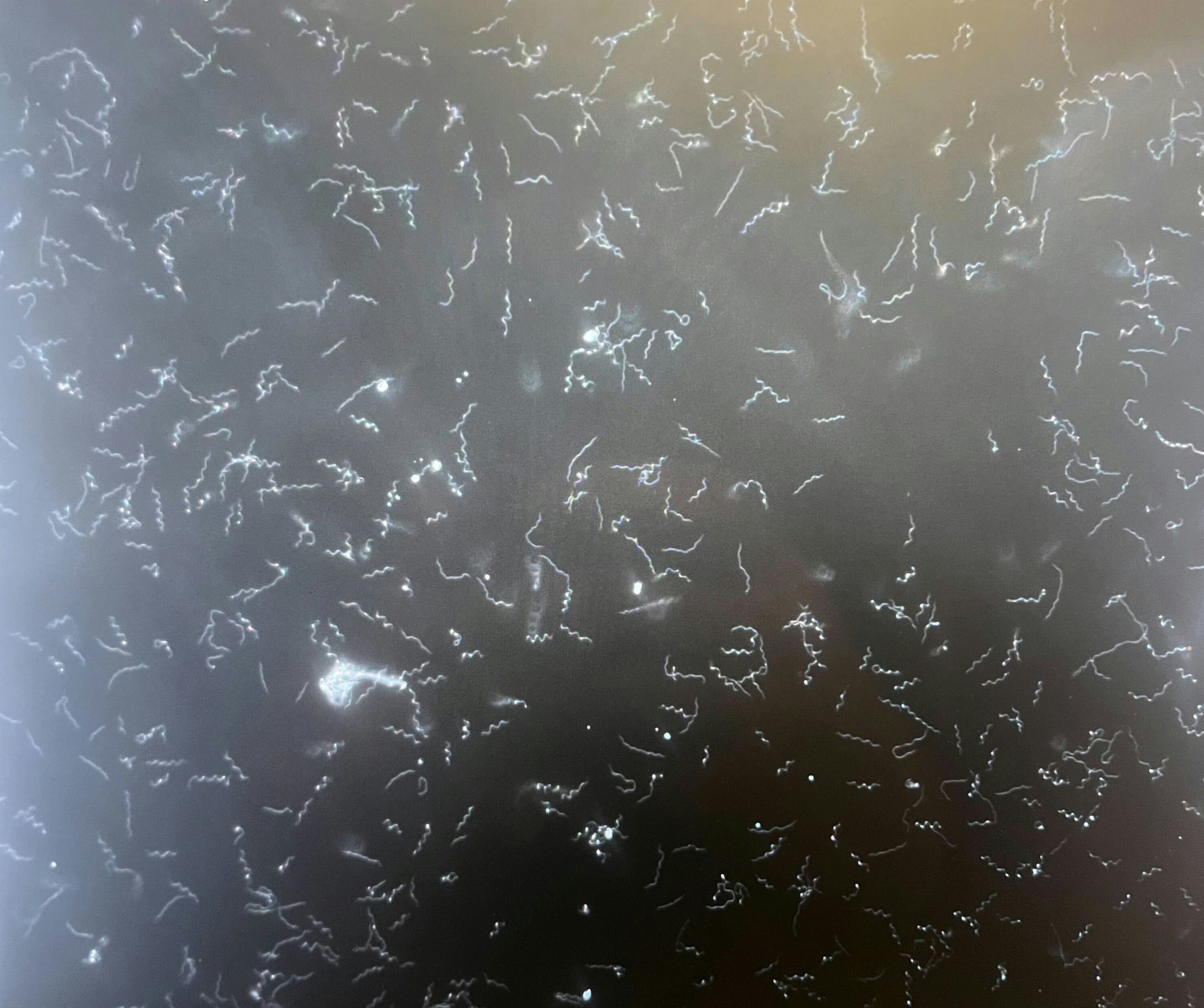
Borrelia burgdorferi, named afer medical entomologist Willy Burgdorfer, is a curious microbe. While most bacterial pathogens can be swiftly dealt with by the immune system, Borrelia burgdorferi evades our in-built defenses using an invisibility cloak of lipid-laden proteins (called lipoproteins) dotting its surface.
We don’t quite understand how the bacteria use these lipoproteins, but some scientists are homing in on that answer by studying Borrelia burgdorferi’s genes. In a study published Thursday in the journal PLOS Pathogens, a team of researchers found that in people with disseminated Lyme disease — where the microbe escapes elsewhere in the body outside the initial tick bite — particularly gnarly strains of Borrelia burgdorferi are genetically endowed with more immune-shielding surface lipoproteins.
“[This] is a basic science effort to try to get the genetic variation that’s present in the Lyme bacteria and to try to understand what the consequences are for clinical disease, among other things,” Jacob Lemieux, assistant professor of medicine at Massachusetts General Hospital and the paper’s first author, tells Inverse.
“I think the value of this genetic information is that it gives us a landscape that’s valuable for the research community to better design diagnostics and vaccines [for Lyme disease].”
“Built like a tank”
When Borrelia burgdorferi enters the skin through a tick bite, it eventually spreads to surrounding tissues and organs like the heart or nervous system unless promptly treated with antibiotics. Because tick bites are hard to miss, and not everyone develops the characteristic bull’s eye rash, about 60 percent of those infected with Borrelia burgdorferi will progress to disseminated Lyme disease within the first couple of weeks, according to the Centers for Disease Control and Prevention.
Ordinarily, our immune systems are equipped to deal with those sorts of bacterial infections. In mammals, one arm of the immune system, called the innate immune response, uses several kinds of molecular alarms and firewalls, one in particular called the complement system. Comprised of over 32 proteins, some of which are free-floating in our body fluids and others bound to the outside of cells, the complement system should be our first line of defense against Borrelia burgdorferi.
“There’s this kind of arms race between complement and Borrelia,” said Lemieux. “Borrelia has a lot of clever mechanisms to disable complement.”
One of those mechanisms involves lipoproteins, of which the bacteria has over 75 different types at its surface.
While there’s been much research to suss out how exactly these different proteins are neutralizing the complement system, Lemieux says relationship isn’t entirely clear. Additionally, how these surface lipoproteins influence how virulent a Borrelia bacteria is at genetic level is another missing piece of the Lyme disease puzzle.
To figure out that genetic aspect, Lemieux and his colleagues gathered over 260 Borrelia burgdorferi samples collected by research institutions in Massachusetts, New York, North Carolina, and Wisconsin and nearly 40 from Slovenia where Borrelia burgdorferi only accounts for a minority of Lyme disease cases in Europe versus a majority in the US. These samples were originally collected over a 30-year period between 1992 to 2021 from patients with disseminated Lyme disease.
Lemieux says sequencing all those bacterial genes was a bit of an arduous task since aside from its central twisted clump of genetic materia contained in a region called the nucleoid, Borrelia burgdorferi contain more than two dozen small circular pieces of DNA, called plasmids.
“Plasmids are really difficult to sequence, they have a lot of repetitive DNA elements that took us some time to figure out,” says Lemieux.
While it was known that most of these surface lipoproteins are encoded in these plasmids, what the researchers found was that more invasive strains of Borrelia burgdorferi had many copies of genes for these proteins, specifically ones belonging to a family of lipoproteins called Erp that past studies have found appear to nix complement.
“We found that the more invasive bacteria tended to have more surface lipoproteins and that they were basically, the best way I can describe it, sort of built like tanks,” says Lemieux. “We think probably [this genetic advantage] enable the bacteria to survive in the bloodstream or in other sites in the presence of innate immune defensese, allowing them to spread and colonize other parts of the body.”
Tackling Lyme disease head-on
While scientists knew these variants existed, Monica Embers, director of Vector-Borne Disease Research at the Tulane National Primate Research Center, tells Inverse, “this study provides more insight into how they differ genetically.”
Lemieux believes the results lay the genetic groundwork for understanding what makes one strain of Borrelia bacteria more virulent and invasive than another and how the genetics reflects regional differences.
“A broader feature [of this research] is that different strains with higher rates of invasiveness seems to be present in different regions at different rates,” he said. “One possibility is that there’s more severe Lyme disease in Northeast US because we have more of these invasive strains.”
Lemieux is quick to point out that surface lipoproteins aren’t the only indicator of what makes one strain of Borrelia burgdorferi more invasive than another.
“More invasive strands seem to be more fortified to withstand host [immune] defenses, that may be one clue as to why they’re more invasive,” he says. “I’m not sure if that’s the only story – they may have other kinds of virulence components on their surface. But as far as we know about the function [of these lipoproteins] that jumps out is their complement disabling funtion.”
The findings may lend to different targets for Lyme disease vaccines, such as the outer surface protein C. While this surface lipoprotein tends to vary a lot from one strain to the next, one vaccine strategy could include multiple variants of outer surface protein C that are regularly updated, like Covid-19 or flu vaccines, or tailored for particular at-risk populations.
Lemieux is hopeful these studies could also lend insight into more efficacious therapies for post-treatment Lyme disease syndrome (or PTLDS), which affects around 10 percent of Lyme disease patients. Currently, there’s no standard care for these people, but with emerging research uncovering a genetic link for PTLDS, there may be a possibility of tailoring treatments to fit a patient’s genetics and the strain of Borrelia burgdorferi infecting them.
“We’re not there yet, but I think this is one clue if we did have strain-specific diagnostics,” says Lemieux.







