Remote health care has the potential to connect patients to doctors safely during shelter-in-place. So why do so many Texans remain disconnected?
By Isabela Dias
July 16, 2020
This story was supported by the journalism non-profit the Economic Hardship Reporting Project.
When Hurricane Katrina finally passed in 2005, Reverend Randy Wells found the New Orleans church he had been leading for eight years, and his house, 10 feet underwater. He was one of the lucky ones.
His uncle’s home in Brenham, a town an hour northwest of Houston where bluebonnets dot the rolling fields in the spring, was a safe place to go, so he and hundreds of other displaced families made the journey to Texas. When they arrived, many found temporary housing in apartments and hotels with help from Faith Mission, a local nonprofit and longtime shelter.
Once he himself was settled in Brenham, Wells joined Faith Mission as a way to give back to the town of 16,000 that had embraced him and his fellow New Orleanians. Years later, in 2014, he became the organization’s executive director, overseeing all of Faith Mission’s services, but it didn’t take him that long to notice a pattern among its shelter population: When he asked newcomers if they had ever attempted suicide or were taking medication for mental illness, three out of four reported a diagnosis but said they had dropped out of treatment. Many seeking shelter also said that they struggled with bipolar disorder, post-traumatic stress disorder, or suicidal thoughts. Some said they had tried to self-medicate with drugs or alcohol after a traumatic life event, losing a loved one, or having a miscarriage.
“During a crisis, folks are going to make sure they have something to eat, money, diapers,” Wells says. “Mental health is the last thing they address, and so they end up in the emergency room, in a psychiatric hospital, or in jail.”
People were falling through the cracks and coming to Faith Mission. “We had well-intentioned volunteers who would say, ‘Pull out the Bible. You just need to believe in God,’” Wells says. “But we just didn’t have clinical staff trained to understand the nuances of mental illness.”
Washington County, of which Brenham is the county seat, had only three psychiatrists and five psychologists as of 2018. With 1 psychologist for every 7,383 people—far fewer than in Travis County, for instance, where the ratio is 1 per 1,347—residents looking for long-term therapy must often drive at least 50 miles to a neighboring county.
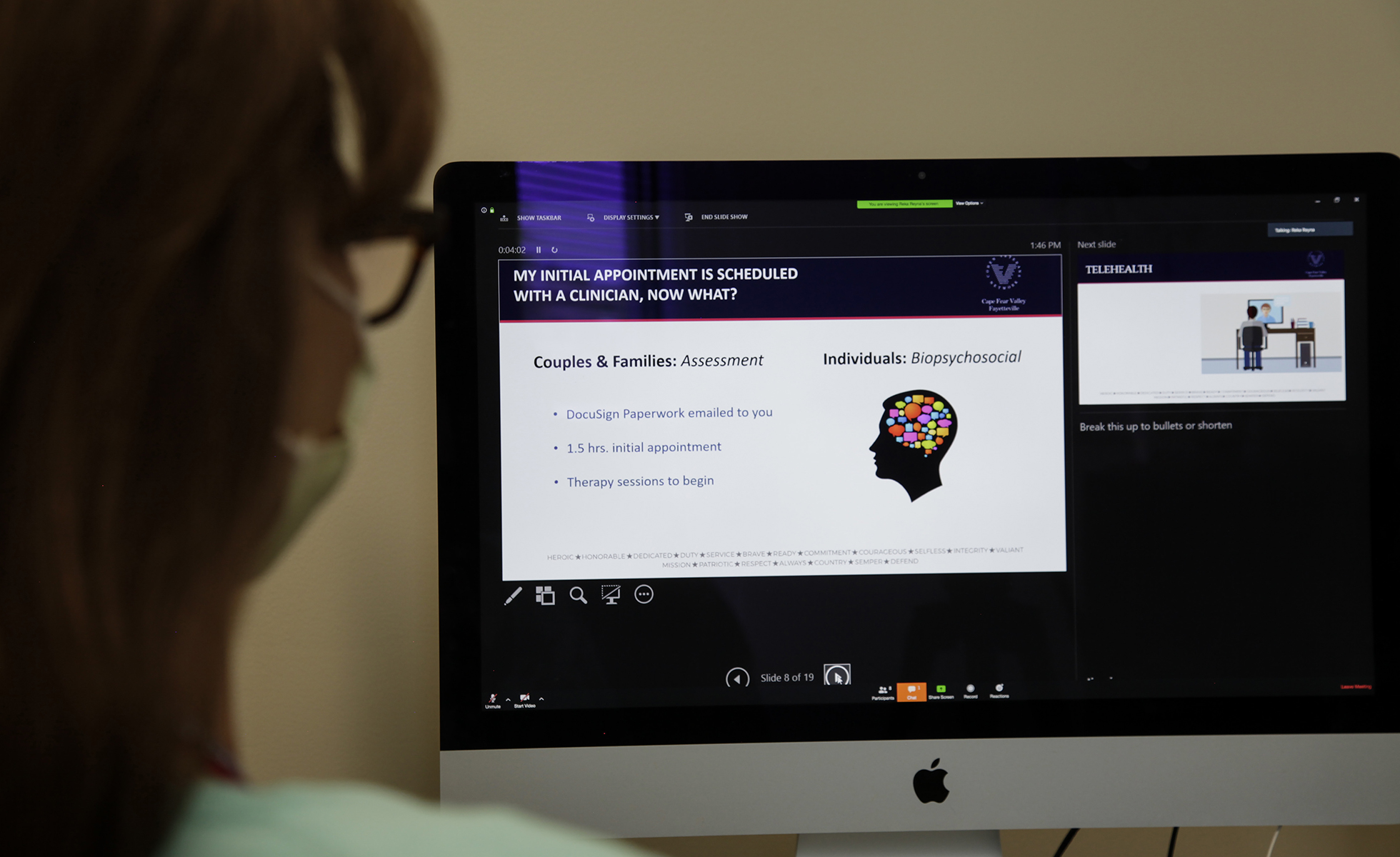
In 2013, Texas A&M University proposed a partnership with Washington County to offer free mental health counseling via video as part of a larger effort to bring services to the Brazos Valley region. But reaching people in their homes, especially in more-rural areas like Burton or Chappell Hill, would have been almost impossible because of limited internet access and bad connections. “Even just cell reception is nonexistent in some of these places,” Wells says. But if patients could go someplace nearby where computers and broadband internet would be freely accessible, they could then attend sessions. Faith Mission stepped in, setting aside a room in its non-emergency health care clinic and installing a dedicated internet line. More than 100 patients have since used the organization’s remote counseling services.
“There was a critical void in our community,” he says. “Now anybody who wants to get mental health help, it’s available.”
Telehealth—or the use of technology to deliver health care services from a distance—has the potential to fill critical gaps in access to health care in rural and suburban Texas. In a sprawling state like Texas, telehealth is sometimes the only alternative to long drives for residents outside of urban centers. But it isn’t possible without broadband, which fails to reach more than 2 million households in the state. Only 69 percent of rural Texans have access to broadband compared with 97 percent of their urban counterparts.
“Patients and doctors are realizing telehealth is a tool to continue to build care even after the pandemic,” says Nora Belcher, executive director of Texas e-Health Alliance, a nonprofit that promotes the adoption of telehealth. “But whether it’s health care or school readiness or emergency preparedness, basic access to the internet is going to separate the haves and the have-nots.”
According to the American Hospital Association, 76 percent of U.S. hospitals use some form of telehealth, yet experts say the adoption of the practice remains generally in its infancy. But that could be changing: During the COVID-19 pandemic, remote medical services have gone from being perceived as a convenient option or a luxury to a necessity.
In Brenham, Faith Mission’s use of telehealth has been a success story, but it still stands as an outlier. So how come so many Texans remain disconnected?
***
When Texas A&M launched its first telehealth counseling clinic more than a decade ago in Leon County, about 60 miles north of the university campus in College Station, there was a clear demand for mental health care. Carly McCord, the director of the university’s telebehavioral health program, remembers how patients reported going to emergency rooms to address panic and anxiety attacks. Decisions to seek medical treatment were often contingent on having access to a car, the price of gas for a round trip, or the ability to take time off work and pay for child care. “We’re talking about really underserved populations,” McCord says. “Kids and adults, uninsured, with a variety of concerns, from mild anxiety and depression to bipolar disorder and schizophrenia.”
The Brazos Valley counts 1 mental health specialist per 7,600 residents; compare that with the statewide average ratio of 1 for every 957 residents. For the 40 percent of the Brazos Valley population living in rural counties, services are almost entirely concentrated as many as 60 miles away. In an area with an average per capita income of less than $25,000 and 20 percent of the population living at or below the federal poverty level, traveling to see a therapist can be prohibitively expensive. A recent community health assessment of the region found that mental health care was the service with the highest percentage of people who needed it but didn’t use it. Almost 80 percent reported putting it off, mainly due to the cost.
Since 2009, McCord and her team have expanded the telehealth services to other parts of the Brazos Valley, including Washington County. But there are still places they can’t reach because broadband access gets in the way.
“We were recently trying to launch new sites and were hoping to work with a particular clinic a little north of us in Rosebud, but we couldn’t because [connection] is just so poor,” McCord says. “And we even use a platform that has one of the lowest bandwidth requirements on the market.”
Rural areas with poor access to mental health and primary care also tend to have poor access to high-speed internet. Service providers often refrain from rolling out fixed broadband infrastructure in less densely populated locations because of high upfront costs and uncertain returns on investments, leaving rural residents at the mercy of unreliable satellite connections or public wifi networks. Even in places where broadband infrastructure already exists, some residents can’t afford a computer or an internet subscription. In Texas, which ranks 38th nationwide in broadband adoption, 1.4 million adults lack the skills or training to comfortably use a computer or smartphone and go online. Almost one-quarter of Texans have access to only one broadband provider. With little competition, private companies often enjoy broad leeway to avoid upgrading services, can impose usage caps, and charge higher fees for poorer connections.
“These services have grown as de facto geographic monopolies, especially in rural areas,” Sharon Strover, a University of Texas media and technology professor says. “The best of all worlds would be for anybody to be allowed to try and provide some kind of internet.”
***
Almost two decades ago, Brian Messman decided to set up a fixed wireless network in Marlin, a tiny town about 40 minutes southeast of Waco. Messman said he and a business partner informed the local provider, Southwestern Bell (now AT&T), of their plans and were told the company had no intention of offering broadband in that area. They used their own savings to roll out towers and started building a subscriber base. But Messman said that as soon as the company saw that there was demand for services, it began to offer broadband and drove Messman out of business. “The phone company will sit and not do anything until they feel threatened,” he says. “They are making money hand over fist right now selling crumbs.”
Messman is now the information technology director of the Falls Community Hospital & Clinic in Marlin. He pays AT&T $65 a month for a 5Mbps connection, one-fifth the minimum speed currently defined as broadband by the Federal Communications Commission (FCC).
“Imagine that you can sit at your home anywhere on the planet, except for Falls County, and stream Netflix and browse the internet on your phone at the same time, and we can barely do one thing at a time over here,” Messman says. Meanwhile, his neighbors in Waco and Temple can get speeds up to 1Gbps for anywhere between $40 and $100 per month.
“[AT&T] are the only game in town, so they can play by their own rules,” Messman says. “We’re an afterthought, and we’re stuck with what we have.”
In the rural clinics where Messman works, about 20 miles north and south of the main hospital in Marlin, the internet connection is even less reliable. Sharing basic information between locations becomes a challenge. The medical staff’s ability to access patients’ records often depends on the weather: If it’s dry and hot, they’re good, but as soon as it starts raining or lightning strikes, the system goes down. “We have to fight it every day, every hour of every day,” Messman says. “We’re at a technological standstill as far as what we can do. If you barely have enough bandwidth to operate day to day, how are you supposed to stream two-way video halfway across the state?”
A recent study by Harvard University found that municipally owned networks offer consumers significantly lower prices—and often higher speeds—than the established service providers. In North Dakota, for example, an association of co-ops and small companies created a statewide fiber network. Now rural residents in the state are more likely to have access to high-speed internet than most people living in urban areas.
Local governments in the Brazos Valley are working with the private sector to build a fiber network with speeds of up to 1Gbps to serve health care facilities across the seven-county region, and hundreds of communities across the country have opted to build or operate their own broadband networks. But local providers are still met with resistance from large corporations and lawmakers. More than 20 states prevent or limit local governments from directly providing internet to residents. In Texas, a law from 1995 aimed at fostering market deregulation and competition among telephone companies bans municipalities from obtaining permits to offer telecommunications services.
Still, some efforts have thrived. In 2017, Mont Belvieu successfully argued in a lawsuit that their broadband infrastructure project shouldn’t be considered telecommunications but rather a utility system and became home to the state’s first city-owned fully fiber-optic broadband. By the early 2000s, the town of Greenville, located about 50 miles east of Dallas, had already built a high-speed internet and cable-TV network through its public power electric utility. With 2019 legislation lifting barriers for electric co-ops to provide broadband services, similar initiatives are likely to crop up.
“There are places in Texas that are never going to get broadband if the cities and the co-ops don’t build them, because companies have to respond to shareholders and that’s always going to limit who they serve and how,” says Craig Settles, an industry analyst and consultant for communities that want to set up broadband and telehealth services. “We’ve got to take the handcuffs off a city’s ability to find a solution.”
In recent years, states and the federal government have worked to extend broadband coverage to underserved and unserved areas. Much like in the 1930s, when the federal government offered grants and loans to electricity and telephone companies to take transmission lines to rural areas, the FCC and the U.S. Department of Agriculture (USDA) have created incentives for service providers to deploy infrastructure to more communities and make subscriptions affordable to low-income households. The two agencies spent a combined $9.1 billion in 2018 alone to expand broadband, largely in rural areas. Earlier this year, the USDA announced a $19 million pilot program to fund infrastructure projects, including a 100Mbps network covering a 385-square-mile area in the Brazos Valley.
Federal dollars don’t always reach the areas with the most need, however. For years, the FCC has based the distribution of grants on a flawed mapping system that relies on self-reported data, allowing companies to overstate their service area so that an entire census block is considered covered if a single household has access to broadband. And a recent report by the Institute for Local Self-Reliance found that major service providers seldom invest the billions of dollars received in the form of subsidies in areas where they have no competition.
Advocates and experts have long argued that telehealth services can help boost broadband in underserved areas. The FCC even said telehealth has the potential to be the greatest driver for higher bandwidth capacity. Now COVID-19 could push telehealth into the mainstream. In a matter of weeks, long-standing challenges and bureaucracies related to reimbursement, state-by-state licensing, and eligibility of services that stood in the way of further expanding telehealth have almost “magically” subsided. In Texas, where the most recent legislative sessions had already introduced bills to promote both broadband access and telehealth adoption, Governor Greg Abbott issued an emergency rule instructing state-regulated insurance plans to pay doctors for telehealth services at the same rate as in-person visits and waived regulations limiting audio-only consultations. Service providers have also stepped up to keep customers connected by promising to temporarily waive late fees and not cut off services.
“Some of these changes will probably go away when the pandemic ends,” Belcher says. “So although we’re not looking at a future that is completely virtual, the in-person footprint is definitely going to shrink.”
***
Since March, Randy Wells has been working up to 12 hours a day, seven days a week, at Faith Mission. In addition to managing the organization’s job skills training, after-school groups for homeless children, clinical services, and other programs, he’s been coordinating the COVID-19 relief efforts, including a volunteer network to buy groceries online for elderly residents and help with paying utility bills. Because the organization relies on funds from events and sales from a thrift shop it operates, it has taken a hit financially and is now more dependent on donations. But Wells and Faith Mission are making it a priority to address mental health problems in the community.
Faith Mission has also been running a COVID-19 help line. In its first six weeks, the line received about 2,000 calls, with questions about testing and symptoms, but also about anxiety, stress, and family problems. “I’d say that 50 percent of the calls are somehow related to mental health distress,” Wells says. If he could find the time to take care of himself, Wells would get a massage or a pedicure, or go for a long drive to feel the wind blowing on his face. “The days have been tough.”
He makes sure to take every opportunity to promote the telehealth counseling clinic, whether it’s through interviews to the local radio station or word-of-mouth. When patients stopped going into the clinic following shelter-in-place orders, many started connecting with counselors via video from home. But Wells knows that’s not an option for everyone—certainly not in households without broadband or where several family members have to share a single computer or smartphone. To get around the digital divide, counselors are changing to audio-only sessions when needed.
“We’ve got to meet people where they are,” he says. “Even though we’re socially distancing, we shouldn’t be disconnecting.”
Read more from the Observer:
Neglected in Care: Long before the coronavirus devastated nursing homes, inadequate staffing in for-profit Texas facilities endangered residents, leading to injuries and deaths.
COVID-19 is Surging in Rural Texas, Threatening to Overwhelm Local Hospitals: ICU beds are limited, medical providers are falling sick, and urban hospitals where small facilities transfer critical patients are running out of space.
Reform vs. Rebuild: Defunding Law Enforcement in Texas: Years of activism and a legacy of police violence are fueling demands to reimagine public safety.







