
You can’t live without vitamins; that’s an absolute no. These macronutrients are the grease to our gears, making sure all our bodily systems are running and operating in mint condition. A deficiency in any one of the essential 13 vitamins can lead to a whole host of health problems, sickness, and possibly death.
During the pandemic, there was one vitamin in particular — vitamin D — that received quite a hullabaloo as a potential therapeutic agent against Covid-19. This was in due part to vitamin D’s influence on the immune system and being potentially protective against respiratory infections based on past research. Notably, when then-President Donald Trump got the coronavirus, his physician revealed that along with a course of the antiviral drug remdesivir and antibody cocktail Regeneron, Trump’s treatment regimen included a vitamin D supplement.
But there’s been a lot of back and forth over whether supplementing with vitamin D actually helps make Covid-19 less severe or even prevents the disease to begin with. And according to two studies published this month in the British Medical Journal, it might not. The two papers, one conducted in the U.K. and the other in Norway, found that vitamin D supplements did not appear to protect against catching Covid-19 or other respiratory tract infections. These findings aren’t a definitive answer to the vitamin D-coronavirus question — both studies have limitations which we’ll get into. But they do raise the importance of continuing research into finding easy-to-implement solutions to keep the spiky virus at bay.
Here’s the background — Vitamin D belongs to a group of fat-soluble vitamins, meaning these nutrients are better absorbed when you eat high-fat foods and are stored in adipose tissue, the liver, and skeletal muscles. Because fat-soluble vitamins stay in the body much longer than water-soluble vitamins that need regular replacement, for the most part, you can have too much of a good thing (aka toxicity) when these vitamins are consumed in excessive amounts.
The human body naturally produces vitamin D (which comes in many forms) after we’re hit with some feel-good sunbeams. The exact mechanism involves ultraviolet B (UVB) energy converting cholesterol, which is abundant in the skin, into an active form of the vitamin called vitamin D2. Dietary supplements come in vitamin D2 and vitamin D3. The latter is slightly more active, therefore more effective, and what most clinicians recommend.

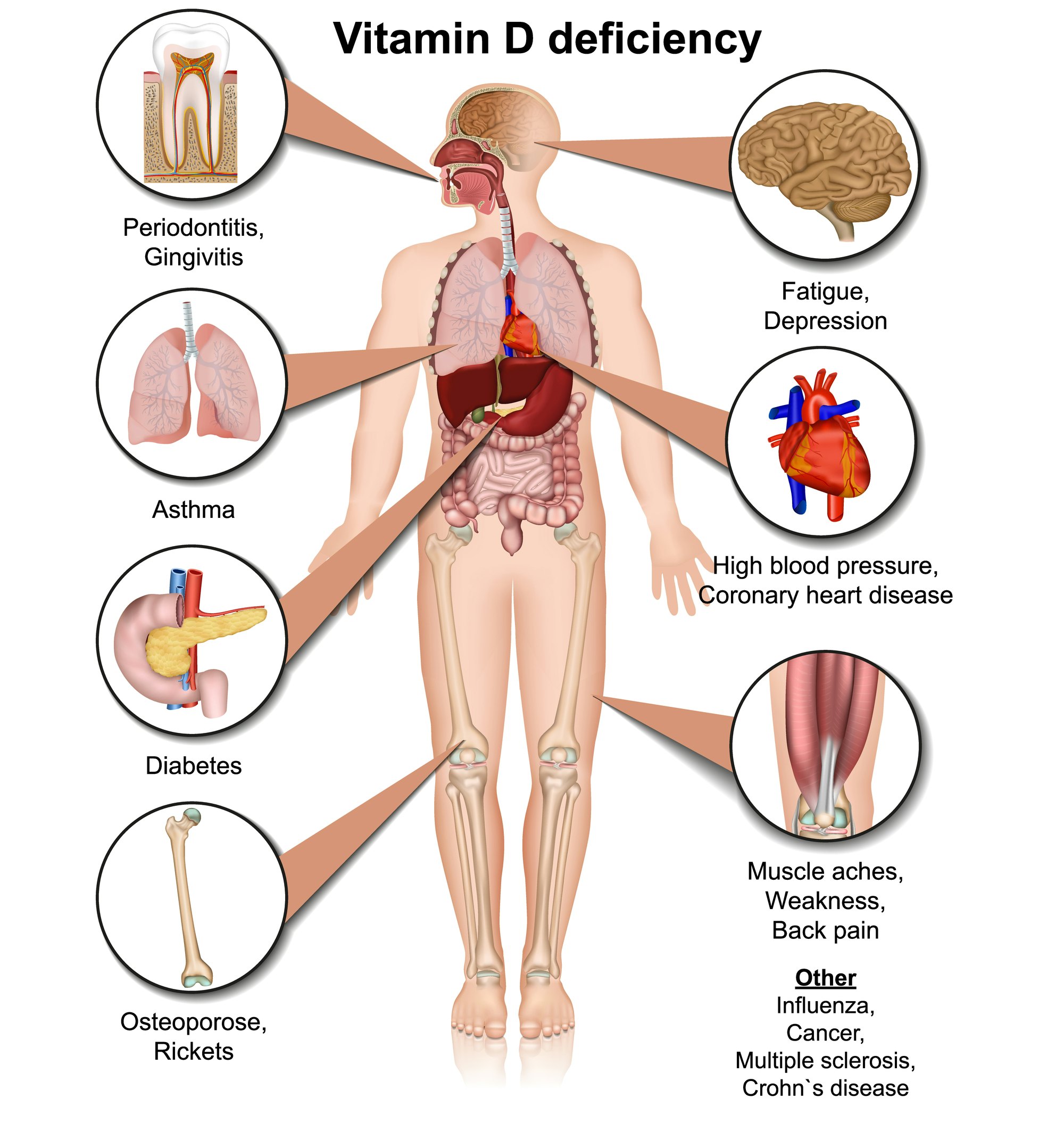
Vitamin D is best known for its role in keeping bones healthy by helping us absorb calcium and phosphate during digestion (thereby preventing osteoporosis). As for its role in immune health, which is where its influence on Covid-19 infection comes in, some studies have shown taking a supplement regularly may prevent autoimmune diseases and metastatic or fatal cancers. Other studies have found that vitamin D may quell inflammation, which may be the link between the vitamin and Covid-19. Additionally, this association appeared to carry some weight as scientists observed high rates of vitamin D deficiency running in tandem with severe Covid-19, especially in Black and Hispanic communities where such a deficiency is highest.
What they did — In the U.K. and Norwegian study, the aim was straightforward: To see if vitamin D, whether as a vitamin D3 supplement or fortified in a teaspoon of cod liver, could prevent Covid-19 infection.
Researchers led by the University of London conducted a phase three randomized, controlled trial enrolling 6,200 volunteers ages 16 years and older from a much larger research cohort called COVIDENCE UK and tested their vitamin D levels. Anyone who had insufficient concentrations of the vitamin in their blood, determined through a finger prick test and defined as less than 75 nanograms per deciliter, was given either a high (3,200 international units per day) or low (800 international units per day) dose of vitamin D3. These individuals, who were mostly women in their 60s, were followed for six months from December 2020 to June 2021.
Up north in Scandinavia, researchers led by a team at Oslo University gave over 34,000 Norwegians aged 18 to 75 years five milliliters of cod liver oil daily (containing 10 micrograms of vitamin D) or a placebo in the form of corn oil. The participants, also mostly women but trending younger (around 45 years old) were followed up for six months as well from November 2020 to June 2021.
What they found — Neither study found vitamin D made a dramatic difference in the number of Covid-19 infections, serious illness (including hospitalizations and any deaths), or other respiratory tract infections between the controls and those taking the vitamin in whichever form.
"Among people aged 16 years and older with a high baseline prevalence of suboptimal vitamin D status, implementation of a population level test-and-treat approach to vitamin D supplementation was not associated with a reduction in risk of all cause acute respiratory tract infection or Covid-19," authors of the UK study wrote.
“Daily supplementation with cod liver oil, a low dose vitamin D, eicosapentaenoic acid, and docosahexaenoic acid supplement, for six months during the SARS-CoV-2 pandemic among Norwegian adults, did not reduce the incidence of SARS-CoV-2 infection, serious Covid-19, or other acute respiratory infections,” the Norwegian researchers wrote in their study.
Digging into the details — Before you go off and chuck your bottle of Nature Made’s D3 in the nearest trash, these two studies do have a number of limitations, the most glaring being vaccination.
In an accompanying editorial, Peter Bergman, a physician and clinical researcher in Sweden’s Karolinska Institutet, who was not involved in either study, said having a sizable number of people already vaccinated (over 35 percent in the Norway study) or undergoing vaccination (from one percent to 89 percent in the U.K. study) may have masked any protective effects of vitamin D.
There’s also the issue of representation in either study. In the UK study, “men, people from ethnic minorities, and those with lower educational attainment were relatively under-represented compared with the general population,” the study authors wrote, thereby affecting the generalizability of their findings.
While the Norwegian study was quite large with over 34,000 participants, most were women, “relatively young and healthy, and 86.3 percent had adequate vitamin D levels… at baseline,” said Bergman. And the fact that cod liver was used, which contains large amounts of vitamin A, also means vitamin D’s ability to regulate the immune system could have been interfered with.
What’s next — While these two studies don’t suggest you forgo vitamin D outright (because you definitely need it for your health and well-being), it’s no substitute for Covid-19 vaccination, at least in individuals with normal levels of the vitamin.
“Importantly, these new trials remain compatible with the two large meta-analyses suggesting that vitamin D supplementation may be beneficial for vitamin D deficient individuals,” wrote Bergman, who also recommended certain groups at risk for low vitamin D, such as those with darker skin, pregnant women, and the elderly with chronic disease consult their physician before supplementing.







