
The dystopian universe of Blade Runner features replicants, or genetically bioengineered people with sci-fi powers, like super-strength and advanced intelligence, that far outstrip any ordinary individual (albeit with a limited lifespan). Their invention is considered a colossal feat of scientific achievement (and the basis for a pretty messed-up society).
But off of the silver screen, we’ve yet to come close to making any organism — let alone a human — entirely from scratch. Until now.
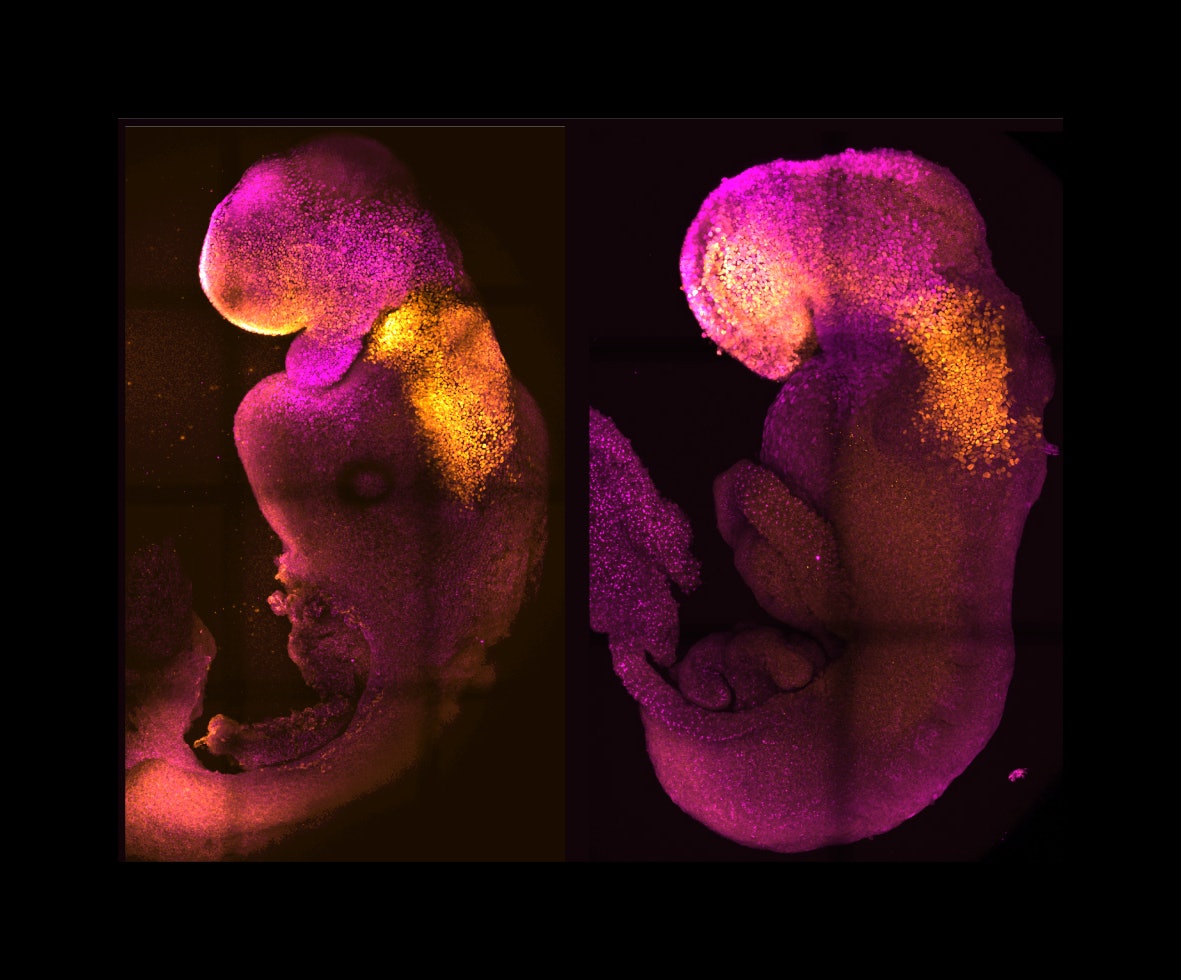
In a study published last month in the journal Nature, scientists in the U.S., U.K., and Israel successfully created a synthetic mouse embryo without using any eggs or sperm. Instead, they used an assortment of stem cells.
Compared to natural embryos maturing alongside them, these lab-grown counterparts developed similar features seen nearly nine days after fertilization, such as a beating heart, a very early-stage brain, and a gut tube — before they abruptly halted growth.
“Essentially, the big question that we are addressing in the lab is how do we start our lives?” said Magdalena Zernicka-Goetz, the study’s lead researcher and a stem cell biologist at the University of Cambridge and California Institute of Technology, during a press briefing.
Peeking into the “black box”
When a sperm fertilizes an egg, the fusion sets off a cascade of changes that cause the single cell to multiply, specialize, and organize into distinct cell types, tissues, organs, and other structures that constitute a complete organism.
For the last several decades, scientists have tried recreating models of embryonic development in the lab to learn how the primordial phenomenon proceeds in real time. But this feat has proven extremely challenging. After all, we can’t just peer into a live uterus in the lab to directly observe the microscopic goings-on.
Specifically, researchers don’t know what exactly happens in the womb between around 14 days and a month into development, says Max Wilson, a molecular biologist at the University of California, Santa Barbara, who was not involved in the study.
During this mystery period, the brain gets built and the heart is laid down. “It’s called the ‘black box’ of human development,” he explains.
This device took seven grueling years of engineering.
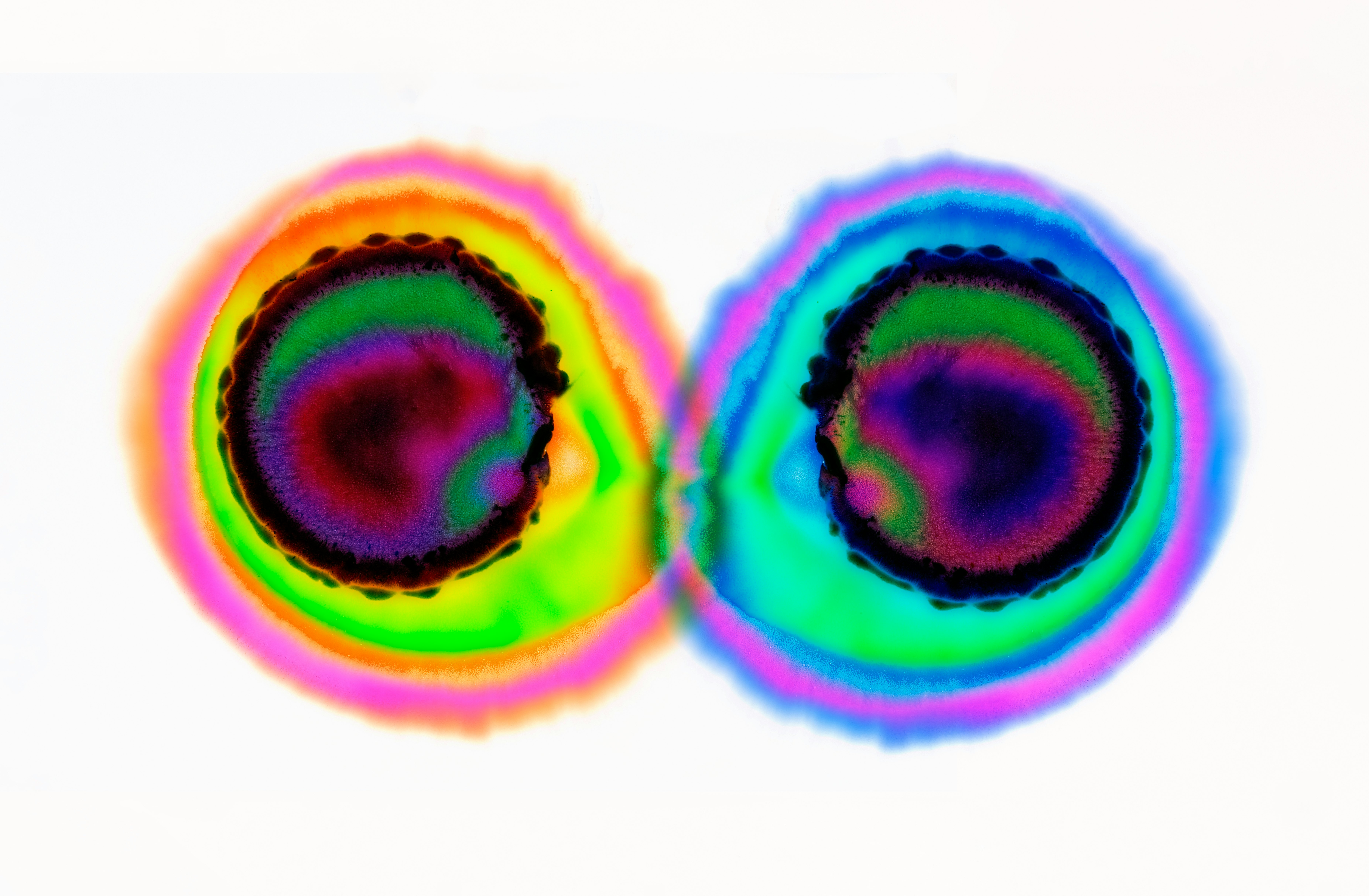
Recent efforts to untangle these mysteries have involved coaxing human embryonic stem cells into blastocysts, a thin-walled, hollow ball of dividing cells that gives rise to the embryo during natural development.
This “blastoid” method didn’t exactly bring scientists closer to seeing how cells self-organize and specialize into organs. But in 2021, researchers at the Weizmann Institute of Science in Israel — who also worked on the new Nature study — developed a sort of mechanical womb (picture an axolotl tank à la Frank Herbert’s Dune).
This device took seven grueling years of engineering. It included an incubator, which floated and spun the embryos in vials filled with special nutrient-rich liquid. Meanwhile, a ventilator provided oxygen and carbon dioxide, meticulously controlling the gasses’ flow and pressure.
With this setup, the Weizmann researchers managed to make stem cell-derived synthetic mouse embryos thrive in their artificial mommy for about six days — until they managed to extend it further, according to a study published earlier this month in the journal Cell.
The embryos underwent gastrulation (when an early embryo transforms into a multilayered structure) over the course of eight and a half days, but then stalled for unknown reasons. (A mouse pregnancy lasts for about 20 days.)
But the experiment wasn’t entirely a dud. It set the mammoth task for the latest study: to show it was entirely possible to grow mammalian embryos outside the uterus.
How to grow a baby
Zernicka-Goetz, one of the authors behind the new Nature study, has spent the last decade investigating ways to develop synthetic embryos. She said her lab only initially used embryonic stem cells to mimic early development.
But in 2018, she and her colleagues discovered that if they tossed in two other stem cells that give rise to the placenta (the organ that provides nutrients and removes wastes) and the yolk sac (a structure that provides nourishment during early development), the embryos were better prepared for self-assembly.
Here’s the thing about science: there’s always competition. After their 2018 Nature paper, Zernicka-Goetz’s team was surprised when the Weizmann group came out with an incubator-ventilator system, along with later experiments that forged embryos without sperm or eggs — just as they were attempting.
But science is also about collaboration. The two groups eventually teamed up to see whether combining their techniques could culminate in the life-creating golden ticket.
The results were impressive: Zernicka-Goetz and her colleagues watched the artificially wombed cells grow into synthetic “embryoids” without any sort of external modifications or guidance.
The embryo model developed a head and heart — parts of the body researchers could never study in vitro.
Compared to the natural mouse embryos that were grown separately, these embryonic mice went through the same stages of development up to eight and half days after fertilization (just like the Weizmann team’s earlier work) which is equivalent to day 14 of human embryonic development.
The embryo model developed a head and heart — parts of the body researchers were never able to study in vitro, said Zernicka-Goetz.
“This is really the first demonstration of the forebrain in any models of embryonic development, and that’s been a Holy Grail for the field,” co-author David Glover, a research professor of biology and biological engineering at Caltech, said during the press briefing.
Zernicka-Goetz’s team also tinkered with a gene called Pax6, which appears to be a key player in brain development and function. After removing Pax6 from the mouse stem cell DNA with the help of CRISPR, Zernicka-Goetz and her colleagues observed that the heads of these synthetic embryos didn’t develop correctly, mimicking what’s seen when natural embryos lack this gene.
In humans, rare mutations or deletions of Pax6 can lead to abnormal development of the fetus and death. They can also spur conditions like aniridia (absence of the eye’s colored part, the iris) or Peters anomaly, which hinders the development of eye structures like the cornea.
A chance for synthetic life?
The detailed glimpse into early embryonic development could be a boon to human health. For instance, it could help scientists grasp why many pregnancies, whether naturally conceived or via assisted reproductive means, fail in the early trimester.
Zernicka-Goetz said the research might also advance regenerative medicine. It could help scientists learn how to make viable, full-functioning replacement organs for a transplant patient using their own stem cells (potentially eliminating the need for lifelong use of immunosuppressants).
Currently, we have a broad sense of organogenesis — or the development of an organ from embryo to birth — but we don’t know all the microscopic steps and cellular interactions that culminate in a fully-fledged, functional organ.
The model system could aid the development of new drugs: It may reveal which medications are safe to take during pregnancy without harming the fetus. Now, researchers can potentially test them out on synthetic embryos, Zernicka-Goetz said.
“This is an advance but at a very early stage of development, a rare event which while superficially looking like an embryo, bears defects which should not be overlooked,” Alfonso Martinez Arias, a developmental biologist at Pompeu Fabra University in Spain who wasn’t involved in the study, said in a press release.
One glaring challenge: While the synthetic mouse embryos appear identical to their natural counterparts, their stalled development at eight and a half days makes it tough to say whether they’d continue to grow right on course.
“This is very strong evidence that we will one day have this power, and it will be possible [to create synthetic life].”
So despite its enormous potential, fashioning synthetic embryos from stem cells just isn’t possible right now.
“This blockade is not understood and needs to be overcome if one desires to grow mouse synthetic embryos past day eight,” Christophe Galichet, a stem cell biologist at Francis Crick Institute in London who also wasn’t involved in the new work, said in the same press release.
Since humans and mice don’t exactly share all the same characteristics when it comes to embryonic development, the next step is to eventually concoct synthetic embryos from human stem cells.
That likely will prove complicated, more so ethically than technique-wise. But Wilson thinks this research marks a major scientific milestone and tool to add to humanity’s technological toolbox.
“This is very strong evidence that we will one day have this power, and it will be possible [to create synthetic life],” Wilson says. “Whether we decide to do that or not because of ethics or even the potential upsides — that’s a question for society at large.”







