
The junior doctors’ strike will lead to caesarean births being cancelled, an increase in the number of mental health patients detained, and issues transferring the critically ill for urgent care, according to leaked NHS documents that show that the impact of the 96-hour walkout will reverberate through the NHS for months to come.
The action over pay, which begins on Tuesday, will compromise critical care and major trauma services, while there will even be a delay to funerals because doctors will not be available to issue death certificates.
Patients were warned on Monday to avoid “risky” behaviour and stay away from A&E if possible, while hospital bosses estimated that 350,000 routine operations were likely to be cancelled.
Hospitals are expecting as few as half the number of consultants to cover junior doctor shifts as during the previous strike, because of “fatigue” among staff and planned leave over the school holidays.
Internal predictions sent to the Department of Health and Social Care (DHSC) last week also warned that low staffing levels in critical care services would affect clinical care for both adults and children, with patients not receiving medicines or assessments on time.
Have you been impacted by this story? email rebecca.thomas@independent.co.uk
There is particular concern over hospitals in the South West, which are experiencing worse staffing shortages along with an increase in demand from tourists.
On Monday, NHS Confederation chief executive Matthew Taylor urged the government and junior doctors’ unions to call in the Acas conciliation service in order to end their stalemate and avoid further “catastrophic” strikes.
Speaking to Sky News, Mr Taylor said: “There’s no point hiding the fact that there will be risks to patients, risks to patient safety, risks to patient dignity, as we’re not able to provide the kind of care that we want to.”
He advised the public to use NHS services in “the most responsible way you can”, and to avoid “risky behaviour” of a sort that could result in a visit to A&E during the strike.
“The health service has to meet high levels of demand, at the same time as making inroads into that huge backlog that built up before Covid, but then built up much more during Covid,” he said.
“That’s a tough thing to do at the best of times; it’s impossible to do when strikes are continuing.”
Junior doctors are set to walk out for 96 hours, with no exceptions applied to any services, including emergency care – although in a letter last week, NHS England said the British Medical Association (BMA) had agreed that, should a major incident occur, the NHS would be able to ask the union to send striking staff back to work.
The medical director of NHS England, Stephen Powis, has warned that the action will have “unparalleled levels of disruption”, with 350,000 operations expected to be cancelled according to the NHS Confederation, which represents hospital trusts. This is double the 175,000 appointments cancelled during the three-day strike in March.
The documents sent to the DHSC last week warned that there could be “significant” and “widespread” cancellations to outpatient services, including for people needing life-saving care, such as cancer appointments and chemotherapy. The effects are expected to outstrip by far the impact of the previous strike.
Mental health services are also expected to be more widely affected this time, with fewer doctors to carry out patient assessments on hospital wards. This could lead to “unnecessary continued detentions under the Mental Health Act”, according to the documents.
There are also expected to be worse delays for mental health patients attending A&E, because of staff shortages. Even in normal circumstances, these patients can be left waiting for days in emergency departments.
With staffing focused on critical and emergency care, there are expected to be delays in doctors signing death certificates, leading to further delays in coroners’ services and funerals.
To try to minimise the impact of the four-day strike, NHS England is planning to move staff working in community care to emergency services.
During the last junior doctors’ strike, hospitals experienced the highest levels of emergency demand they’d seen this year.

A checklist sent by the BMA to the NHS for emergency situations includes questions about the pay rates hospitals have offered doctors.
According to the list, which has been seen by The Independent, hospitals are being “forced” to comply with minimum rates set by the BMA for consultant cover, which can be as high as £260 per hour.
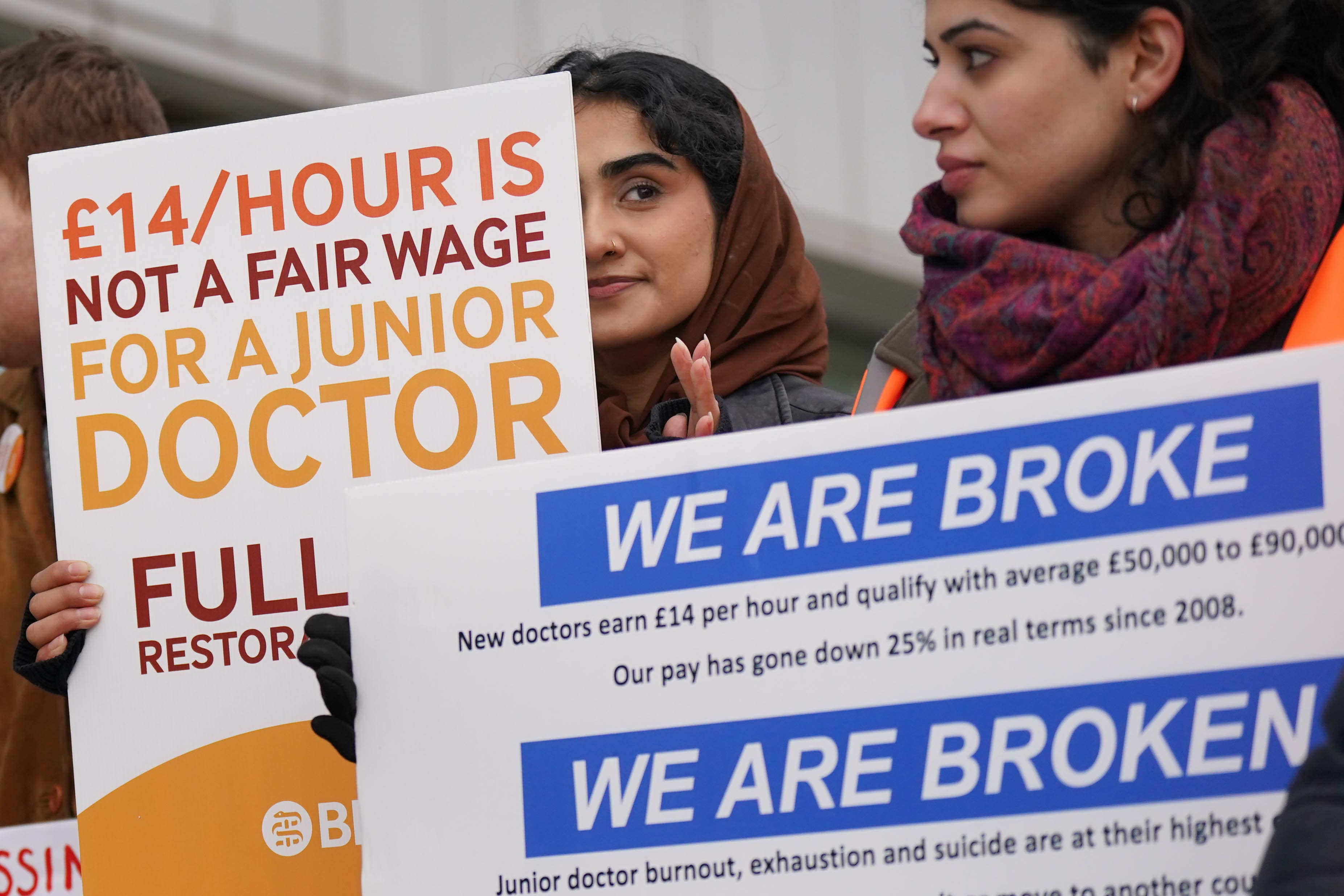
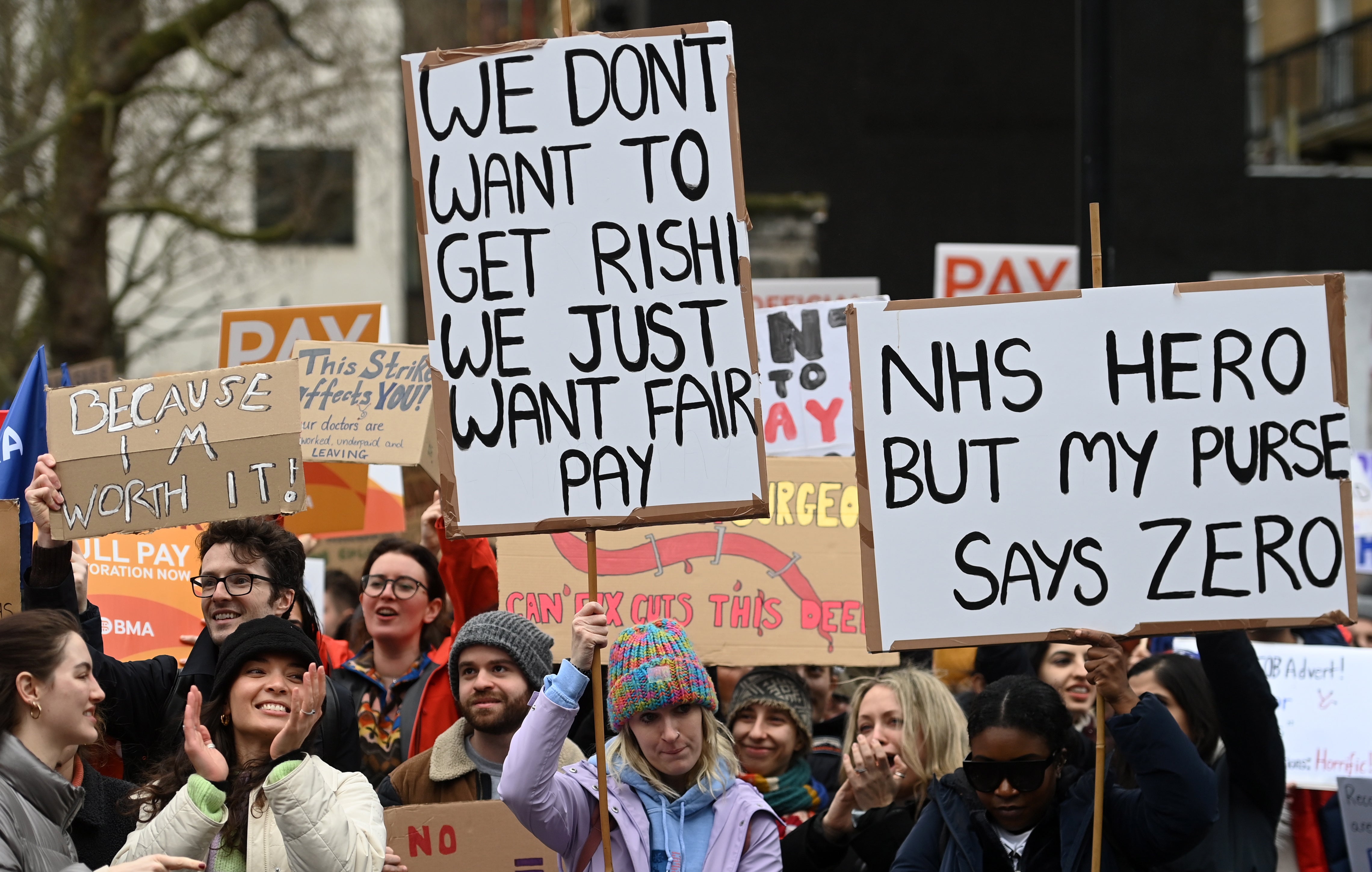
The BMA has asked the government to address a 26 per cent real-terms pay cut to junior doctors’ wages since 2008-2009, which would require the government to sign off on a 35 per cent pay increase this year.
Health secretary Steve Barclay has described the demand as “unrealistic”, and said that the strikes had been planned to “cause maximum disruption”.
“This demand is widely out of step with pay settlements in other parts of the public sector at a time of considerable economic pressure on our country,” he wrote in The Sunday Telegraph. “A salary hike of this size would see some junior doctors receiving more than an extra £20,000 a year,” he said.
“I recognise their hard work and dedication. But it is deeply disappointing that this industrial action has been timed by the British Medical Association Junior Doctors Committee to cause maximum disruption to both patients and other NHS staff.”







