
Although obesity has been recognized as a disease by the World Health Organization (WHO) since 1948, its identity as a disease may not be widely perceived the same way as other health conditions.
People living with obesity are less likely to receive dedicated care for that condition, in contrast to patients with other diseases, such as cancer. However, obesity and cancer have several similarities. This is of global crucial importance, given the dramatic increase in numbers of affected adults and children, including in Canada.
Obesity is a disease
Like cancer, or other medically recognized diseases, obesity should be seriously considered as such by public opinion. Not only is obesity itself a disease, but it can also contribute to the onset and progression of cancer and other diseases, such as diabetes, atherosclerosis, heart attack and stroke.
The disease of obesity affects people in several ways:
Mechanically: Obesity imposes an excessive pressure on the bones and the joints, as well as internal organs. It can also potentially cause airway obstruction that can lead to obstructive sleep apnea.
Biologically: Obesity can lead to osteoarthritis, for example, and it presents with inflammation and dysregulated secretions by dysfunctional fat tissue cells.
Obesity can also result in abnormal fat deposits on vital organs, which seriously alters the whole organism’s homeostasis, or biological stability.
Psychologically: Patients with obesity may face difficulties in accomplishing daily activities; even simple things such as tying their shoelaces may be a challenge. This is further worsened by social media’s deep influence and promotion of a presumed “ideal” unrealistic body shape image, which stigmatizes patients with obesity.
There is also evidence that obesity is accompanied by brain inflammation and increased risk of mental health conditions such as major depressive disorder and anxiety.
Common characteristics of obesity and cancer
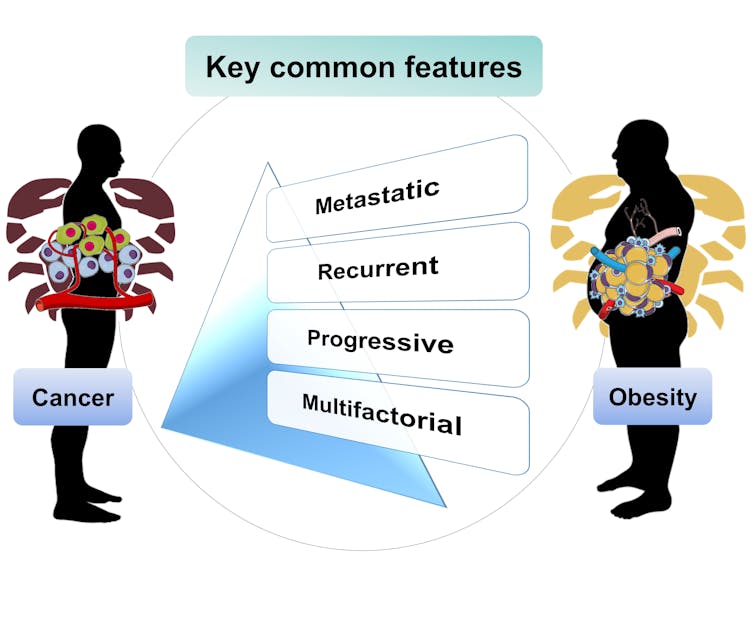
Obesity shares several major features with cancer:
Multifactorial grounds: Both diseases present no single known cause, which can make prevention and treatment challenging.
Obesity is not simply due to individual lifestyles of high-calorie consumption or low levels of physical exercise, since the balance between energy intake and expenditure can be tipped in either direction by genetics, the environment as well as other factors that are not completely understood.
Metastasis: Like cancer, obesity can involve metastases, meaning that the disease can spread to other parts of the body.
In the case of obesity, this takes the form of ectopic fat deposits, which occur when adipose (fat) tissue cannot store all of the excess triglycerides, a type of lipid, or fat. Triglycerides then accumulate beyond their normal locations, including around organs. In obesity, fat can be deposited on the heart, the liver, in blood vessels and even the brain. These deposits can alter vital organ function and have devastating effects on an individual’s health.
Progressive development and stages: Obesity, like cancer, can develop progressively to reach advanced harmful stages. One of the reasons why people may consider obesity as a less serious illness than cancer is that they may pay more attention to the stages of cancer.
In fact, both obesity and cancer might advance progressively in the absence of proper diagnosis and intervention. However, deaths that originate in obesity are most often attributed to potential consequent diseases (such as cardiovascular ischemic events or even cancer) and neglect the pivotal impact of obesity.

Recurrence: Those who recover from obesity can experience recurrence of the disease. A good example is seen in The Biggest Loser TV series. Contestants who lost weight on the show later regained it.
Obesity recurrence is often referred to as “yo-yo” effect. However, “recurrence” is a better term that should replace yo-yo, since it more seriously emphasizes that obesity is far from a game. In fact, certain patients struggle deeply to curb uncontrollable weight regain.
Read more: The obesity epidemic is fuelled by biology, not lack of willpower
As illustrated by the tale of the Emperor’s New Clothes, people’s perceptions can be erroneous. Often, perceptions of obesity do not reflect its serious threats to health. Obesity is scientifically proven to be a disease, and internationally recognized as one. The mirroring of its features with cancer reveals its inherent morbid potential.

Obesity is a disease because it can cause deterioration of several aspects of health. WHO defines health as “a state of complete physical, mental and social well-being and not merely the absence of disease and infirmity.”
Even though obesity shares numerous morbidity characteristics with cancer, it does not get the same society-wide recognition as a disease, and people with obesity may be less likely to get the help and treatment they need. There is an urgent need to reshape the way obesity is viewed.
The authors receive funding from the Canada Excellence Research Chair on the Microbiome-Endocannabinoidome Axis in Metabolic Health (CERC-MEND; Chairholder Prof. Vincenzo Di Marzo), which in turn is funded by the Canada First/Apogée program of the Tri-Agency of the Canadian Federal Government.
Cristoforo Silvestri receives funding from the Canada First Research Excellence Fund through Sentinelle Nord of Université Laval.
This article was originally published on The Conversation. Read the original article.







