When you become a mother, everything about you changes, even your DNA. In a process called foetal microchimerism, “zombie cells” from the baby cross the placenta and circulate through the mother’s body, lodging in her organs and tissues like pregnancy souvenirs.
For decades after pregnancy you carry these cells proving that the maternal/infant ties that bind extend much deeper and for much longer than the umbilical cord has us believe.
This isn’t the kind of news you’re likely to receive in your antenatal appointments but it’s the kind of information that affirms the seismic shifts you’re surrendering to. In a world focused on success and productivity, we often fail to acknowledge the most productive thing that any of us can do: reconfigure to grow a new life (and a marvellous, albeit temporary organ) and then produce bespoke milk to sustain it.
The language of motherhood is one mothers and writers are constantly exploring because many of us find it difficult to explain how it feels; the intimacy and enormity of it. On the flipside, we’re often labelled with language that’s hard to hear; derogatory words that settle in our minds and prompt us to question our growing, birthing and mothering abilities.
Mum-shaming, it seems, starts well before the baby is born.
For instance, if you’re having a baby over the age of 35, your pregnancy will be deemed geriatric.
After receiving two positive lines on a pregnancy test, you may become the statistic; one in four pregnancies in Australia end in miscarriage; a silenced and often grief-filled experience, marred by a label that presumes you’ve mistakenly left your precious cargo behind.
If you’ve ever had morning sickness you’ll know that it’s a persistent beast that hangs around well after lunchtime, and often lingers 24/7 for weeks or months on end. Let’s call it what it is – nausea and vomiting in pregnancy (NVP) – rather than belittling its severity by fitting it into a neat timeframe.
For some women, labour may start much earlier than it should, usually spurred on by the silent shortening and thinning of the cervix – the neck that joins the womb to the vagina. A cervical stitch may be inserted, bed rest prescribed and the official diagnosis of incompetent cervix added to your file; a term that adds insult to injury at a time that is acutely dangerous for the baby and frightening for the mother.
Once you feel the distinctive twinges of the first contractions and settle into the ebb and flow of labour, you’ll know there’s no going back now. But labour can slow, and sometimes halt, typically when you feel anxious or fearful because the fight or flight response stops the flow of oxytocin, the shy hormone responsible for driving contractions.
Sometimes, even with oxytocin flowing (natural or synthetic), the cervix doesn’t dilate, and your hospital notes may read: failure to progress.
If you do dilate and you reach the second stage where you’ll bear down to birth your baby, it may be hard to know how to push, or your baby may be in a position that doesn’t make the descent a simple one. In this case you may need instrumental assistance and sometimes the noted reason for this will be: poor maternal effort.
Regardless of how you birthed, your uterus will continue contracting in a process called involution, vital to ease blood loss and ensure maternal wellbeing. The uterus – the organ that secretes milk to nourish the growing embryo in the first 11 weeks of gestation and then stretches to 40 times its size in pregnancy – comes from the Greek word, hystera – the origin of the word, hysteria.
If you choose to breastfeed but you don’t produce enough milk to sustain your newborn, you may be diagnosed with: insufficient glandular tissue.
These terms are medically accurate but there’s no denying they’re also quite insulting. Medical terminology is always evolving and there have been positive changes in some maternity sectors with the move away from terms that suggest the birthing woman is at fault or blame. At a physiologically vulnerable time, mothers in pregnancy and postpartum need language that acknowledges their monumental experience and simultaneously gives them hope.
Birth is the main event, and so it should be, but what happens afterwards is an intimate and confronting period of becoming because everything has changed and nothing will be the same again.
Matrescence is to mothers what adolescence is to teenagers, a transitional period of hormonal and biological upheaval that’s innately awkward. It’s coupled with a shifting identity; the way you see the world and the way the world sees you is markedly different.
It nods to the brain changes that occur in pregnancy – the most significant of any human experience – where the brain effectively fine-tunes itself so it’s prepared for the period of rapid learning of new motherhood. The only other time this occurs is in adolescence.
Matrescence flips bounceback culture on its head and sparks a sense of wonder alongside the reassurance of understanding.
Knowing what matrescence is and what it means is like coming home. It says to new mothers: “This isn’t supposed to be easy, you’re going to feel untethered and uncertain, you’re not supposed to know all the answers because you’re learning.”
It dismisses the ideology of the martyr mother and instead offers us the grace to be good enough. It’s the comfort in the dark of the night when, through milk and tears, you start to make sense of yourself and the person you’re becoming.
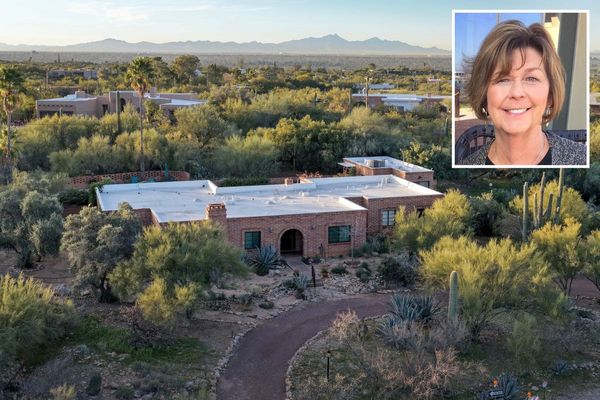
• Jodi Wilson is a postpartum doula, mother of four and author of two books: Practising Simplicity and The Complete Australian Guide to Pregnancy and Birth