Scientists have developed a device that could potentially prevent skin infections by zapping harmful bacteria with electricity.
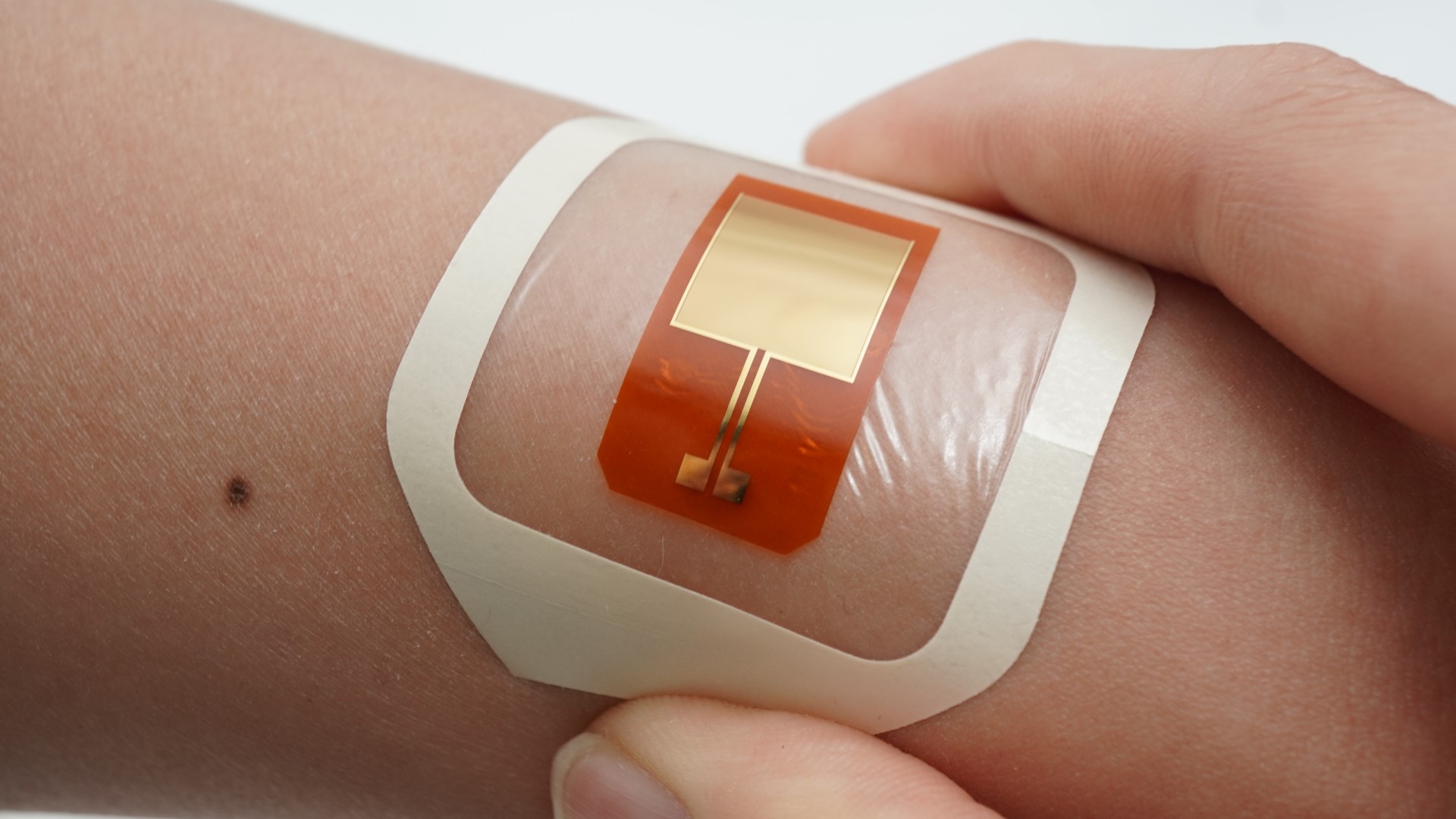
The device — named Bioelectronic Localized Antimicrobial Stimulation Therapy (BLAST) — is a patch that sticks to the surface of the skin and delivers a very weak, harmless electrical current via electrodes, stopping disease-causing bacteria in their tracks.
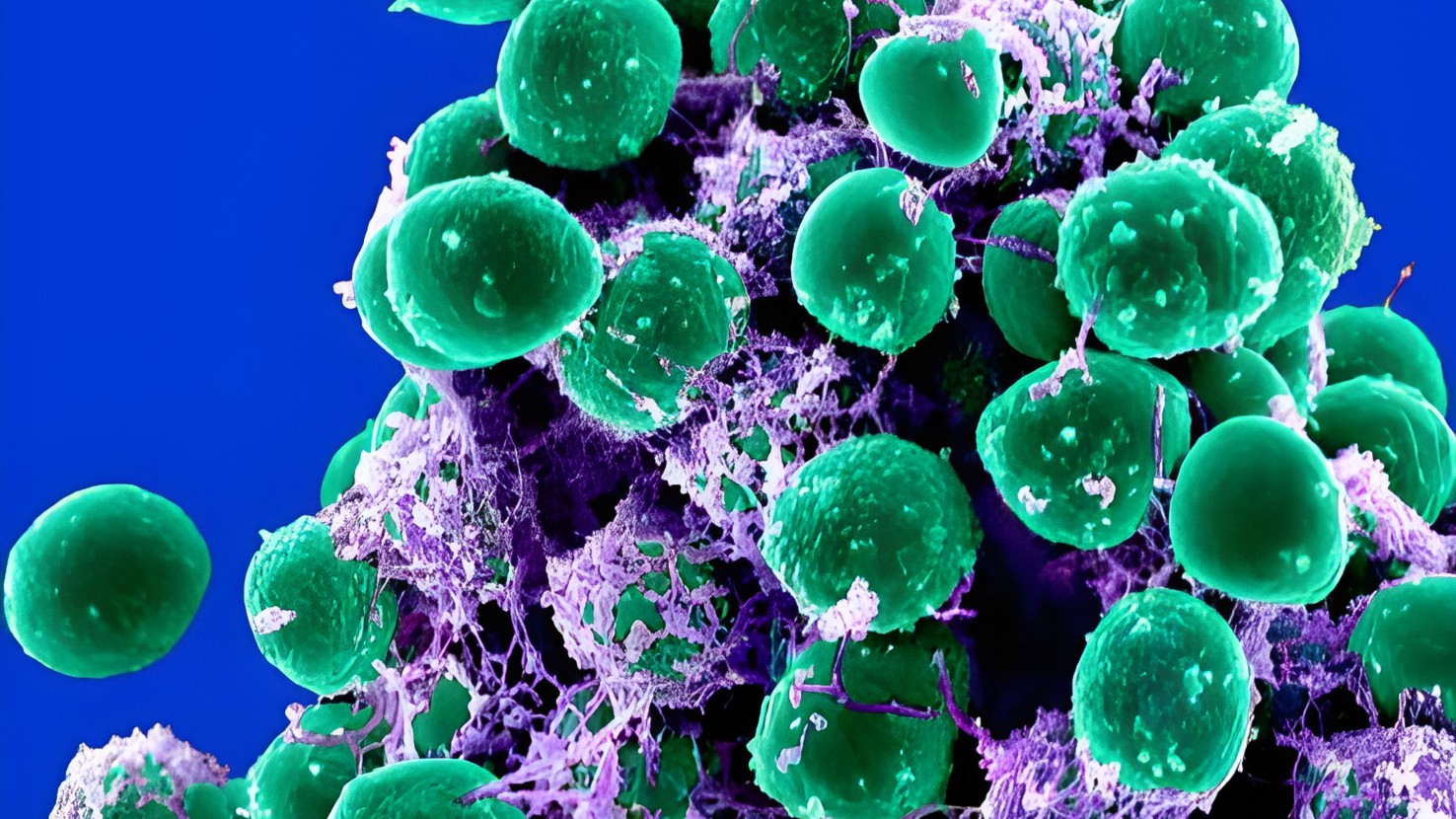
In a new study, researchers tested BLAST on pig skin, which is often used as a stand-in for human skin in preclinical experiments because of its similar structure and function. On this skin, the researchers released Staphylococcus epidermidis bacteria, which commonly live on healthy human skin,
Typically, these bacteria keep the growth of harmful microbes on the skin in check and even help to promote wound healing in the skin. However, if S. epidermidis bacteria inadvertently end up in the body — for instance, via a contaminated medical device, such as a catheter or IVs used to deliver drugs — they can spark dangerous infections.
Related: When not causing breakouts, acne bacteria may strengthen the skin's protective barrier
Experiments in the new study showed that S. epidermidis does something that the researchers call "selective excitability." In response to electricity, the bacteria turn down the activity of genes that enable them to assemble in thick, slimy layers, known as biofilms. Biofilms allow bacteria to better stick to, and thus colonize, surfaces of the body.
But S. epidermidis only respond to electricity when their surrounding environment is acidic. Healthy skin is mildly acidic, but chronic wounds are usually alkaline. For that reason, the researchers ensured that BLAST would make the skin below the patch acidic by adding a special hydrogel to the patch.
During testing, the device delivered 10-second electrical pulses to the skin every 10 minutes for 18 hours. Each pulse of electricity was around 1.5 volts — around the same voltage that is delivered by pacemakers used to regulate a person's heartbeat. The device significantly decreased the amount of skin covered by biofilms and reduced the total number of S. epidermidis cells nearly tenfold, compared with untreated skin.
BLAST had a similar antimicrobial effect when applied to the surface of a catheter. This hints that it could theoretically be used as an additional sterilization measure before such devices are used.
These findings, published Thursday (Oct. 24) in the journal Device, offer early hints that the patch could be useful in medical settings. However, future studies need to show that similar effects are seen in living animals' skin and in humans' skin. If the patch clears those tests, it could be used to help prevent bacterial infections without the need for doctors to preemptively prescribe antibiotics, Bozhi Tian, study co-author and a professor of chemistry at the University of Chicago told Live Science in an email.
Cutting down on antibiotic use could reduce the risk of bacteria developing resistance to the drugs, which is a major public health concern.
The team will now investigate whether other species of bacteria respond to electrical stimulation in the same way that S. epidermidis does. If they do, that could expand the clinical utility of devices such as BLAST.
Considering that an array of bacteria live on our skin, singling out one species at a time for testing may not accurately predict how the device works in humans. This is likely something that the researchers would need to consider in future experiments.
Going forward, the team aims to test BLAST in animals before hopefully moving on to clinical trials with people. If the device is proven safe and effective, they believe it could reach the market in around five years, Tian said.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!







