
Richie Goonan knows that when faced with a drug overdose, every second counts.
But Goonan, who leads the community health team at the non-profit Youth Projects, says his frontline workers are hampered by a legal risk that slows them down when responding to an overdose.
Despite Victoria last year joining a federally funded program that expanded access to naloxone, a lifesaving overdose-reversal medication, frontline drug workers are met with a legal hurdle that prevents them from administering it without first calling triple zero.
If they face litigation due to attempting to save a life by administering naloxone, they may not be covered by any indemnity scheme if they have not spoken to an emergency services operator first.
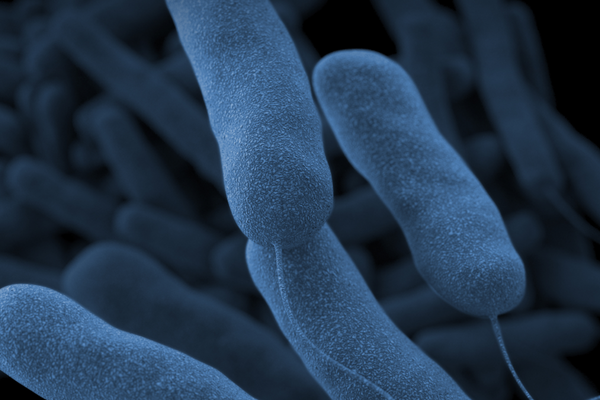
Health experts are warning about the looming threat of strong synthetic opioids, called nitazenes, to Australian drug users, shining a light on the importance of access to naloxone to treat overdoses – with researchers calling for more Australian pharmacies to stock the drug.
Last month police confirmed that a synthetic opioid had been detected in the bodies of four people found dead in Melbourne in June.
Naloxone – available as an injection and nasal spray – can rapidly reverse the effects of an opioid overdose or an adverse reaction.
But Goonan says a nurse outreach worker at his service spent two minutes on hold with emergency services while trying to help someone experiencing an overdose.
“Two minutes is an extremely long time when you’ve got someone with really shallow breathing, lips going blue,” he says.
Such a delay could be the difference between receiving “a lifesaving drug in a timely fashion” and “death or permanent harm”, Goonan says.
“Naloxone is a safe drug to use with the side-effects in the literature being very rare,” he says.
Under Victoria’s good Samaritan legislation, it is legal for a non-medically trained bystander to administer naloxone to a person to treat a potentially fatal overdose. The drug is available to members of the public for free and without a prescription from drug harm support services under Victoria’s take-home program. This year the Allan government announced that it would also trial naloxone vending machines.
But while members of the public can administer it straight away, non-clinical frontline workers must “call 000 as a priority and tend to a person in need of assistance in accordance with the advice of the emergency service operator”, the operational guidelines for Victoria’s take-home naloxone program dictate.
Goonan says there “doesn’t seem to be much sense” in forcing trained providers of emergency care to call triple zero before administering naloxone while members of the public are not required to do so.
One Victorian frontline outreach worker for a needle and syringe program, who requested anonymity, says that before the guidelines were published, he administered naloxone to someone without medical guidance.
“There wasn’t a nurse there and I’m familiar and comfortable in using it,” he says. “There was no reason for me to wait. I knew what I was doing. I knew that it was appropriate.
“I feel very anxious about discovering somebody that is in an overdose situation whilst I’m at work and knowing that if I was to administer it, I’d be doing that knowingly … outside of the legal guidelines.”
The non-profit community health organisation Cohealth’s policy is for non-clinical staff to call triple zero if a clinician is not available when an overdose occurs.
Sione Crawford, the chief executive of the non-profit Harm Reduction Victoria, says the Department of Health last year informed health providers that non-clinical staff who administer naloxone risk not being covered by professional indemnity insurance if an adverse event occurs.
Crawford says sometimes outreach workers are in areas of poor mobile reception or come across someone requiring an immediate response.
“[With] the advent of nitazenes and really potent synthetic opioids, we’re also thinking some of those overdoses can happen in 30 seconds rather than four or five minutes,” he says.
“We always say call triple zero. It might work in 80% of situations … Sometimes calling triple zero can take 90 seconds and that can be life-threatening.”
Last month a synthetic drug 100 times more potent than heroin was found in cocaine being sold in Melbourne, prompting a warning from Victoria’s health department. It suggested users carry naloxone.
There were 549 drug overdose deaths in Victoria in 2022, equating to 1.5 deaths a day, according to the latest data from the state’s coroner’s court. Between 2013 and 2022 the number of overdose fatalities increased by 44%.
Chris Christoforou, the chief executive of the Victorian Alcohol and Drug Association, says the legal hurdle faced by frontline staff is “mind boggling”.
“It doesn’t make sense if the state is expanding access to naloxone, including through 24/7 vending machines, but those on the frontline, working with the drug-taking community, are hamstrung in terms of being able to respond to an emergency,” he says.
Guardian Australia understands that the Department of Health is aware of concerns about indemnity and insurance coverage for the administration of naloxone. It is understood to be investigating the issue.
A Victorian government spokesperson said any member of the public could administer naloxone in response to a suspected opioid overdose but it was always recommended to call triple zero in an emergency.
“We take a health-led approach to drug harms which is why we are making it easier for Victorians to access the life-saving overdose reversal medication, naloxone,” the spokesperson said.



.jpg?w=600)


