Magnets to treat depression? It may sound bizarre, but this treatment is now available on the NHS. It’s called transcranial magnetic stimulation, or TMS.
People who have tried antidepressants but they haven’t worked, may be offered TMS. It involves zapping areas of the brain associated with depression with pulsing magnetic fields.
Treatment usually involves daily half-hour sessions five days a week for two to six weeks.
TMS is not just used to treat depression, it has been used as a diagnostic tool for multiple sclerosis and motor neuron disease. And its effectiveness in treating mood disorders, such as depression and anxiety, has been under investigation for more than 30 years.
It works by sending a magnetic pulse into the brain through a device placed on the skull.
Developing the right device
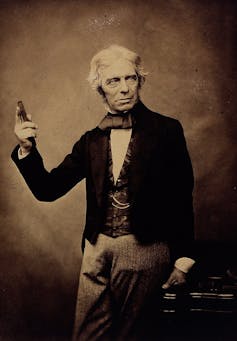
So-called “refractory depression” – depression that does not respond to antidepressants or talk therapy – can be effectively treated with electroconvulsive therapy (ECT). But ECT is fairly invasive, sending bolts of electricity through the skull and into the brain. With TMS, an electrical change in the brain happens because of the magnetic field happening outside of the skull. This is called electromagnetic induction and was discovered by Michael Faraday in 1831.
Over the next century, scientists and doctors such as Jacques-Arsèn d’Arsonval and Sylvanus P. Thompson created devices that sought to artificially stimulate the nervous system, the former for an early defibrillator device and the latter to stimulate the brain. But they were so bulky and the amount of power needed to produce the rapidly changing magnetic field that was required made their development difficult.
It wasn’t until 1985 and the work of medical physicist Anthony Barker at Sheffield University that led to the creation of a compact, relatively inexpensive device that allowed scientists to stimulate 1cm³ area of the brain at time intervals of their choosing for fractions of a second. It is safe and is applied while the patient is awake.
The technique is used to treat depression and anxiety in two specific ways. Sending repetitive pulses into the brain at different frequencies can have different effects.
In depression, we know that activity is low in the left prefrontal cortex – the area of the brain that is important in planning and thought processes. So using a higher frequency pulse switches on those neurons to help them work as they should, thus alleviating the depression symptoms.
In contrast, the prefrontal area on the right side of the brain, which is known to be overactive in cases of anxiety, is treated with lower frequencies to calm the activity in that area.
Using this effect of changing how neurons talk to each other (called neuroplasticity), it is hoped that with regular treatment, symptoms will be alleviated.
The treatment is administered as the patient sits in an armchair and feels something akin to a light tapping on the skull.
Safe, but long-term results are needed
A review of TMS for treating depression found mixed evidence and called for longer-term studies. But it is clear that there is benefit for people with refractory depression, and it is safe in older adults and pregnant people.
TMS is safe to administer to those who do not have metal, such as aneurysm coils, metal dental appliances or non-removable piercings in their head or metal-containing pigments on their faces. But it is not advised for people who have epilepsy.
The treatment has several advantages over ECT. With TMS, the patient does not need to be anaesthetised; they do not experience a seizure, and they do not have memory loss after the treatment.
Using TMS in more clinics will provide scientists with more data to determine when it works and for whom, and what protocols are optimal. For example, TMS may have greater and longer-lasting benefits when paired with cognitive behavioural therapy (a type of talk therapy) – as has been shown with antidepressants combined with CBT.
But it is certainly a technique – forged in the fire of cognitive neuroscience – that can have a great effect on those desperate for help.
Amanda Ellison does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
This article was originally published on The Conversation. Read the original article.