This is part II of a two-part story on the Spanish flu virus. Read part I here.
The United States Centers for Disease Control and Prevention (CDC) is the apex organisation in the U.S. on matters of public health and safety. Research on any new infectious agent must be first approved by the CDC. But in 2005, the CDC received an application for study on a very old infectious agent.
The researchers in question wanted the body’s approval to recreate a deadly pathogen – one that had not infected anyone since 1920. Despite the serious risk to the public, the CDC scientists carefully reviewed the application and granted permission to perform the requisite experiments necessary, because they deemed the experiments the researchers had proposed to be sufficiently important.
The applicants wanted to recreate the H1N1 influenza virus – which had killed around 50 million people in an outbreak in 1918 – from its genetic material.
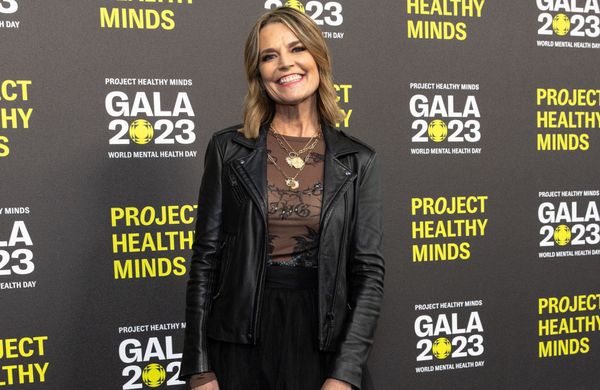
Terrence Tumpey
Influenza viruses are almost always circulating among humans. The nature of the virus means that every year, the virus’s genetic material undergoes some minor changes, rendering it a little different from the virus of the previous year. So scientists have to guess which changes are likely to survive the next year, and design or update their vaccines accordingly.
An influenza virus can also infect birds, pigs, horses, and other domestic animals. It can assort the types of the two genes it contains – haemagglutinin (H) and neuraminidase (N) – in these animals to generate a new virus altogether, some of which may infect humans. All these complications ensure that designing an effective vaccine for influenza remains challenging.
When the CDC received the application for the 1918 H1N1 virus revival, vaccine efficacy was a meagre 10%.
The CDC, realising the value of the proposal, installed special security measures. Only one man, Terrence Tumpey, was authorised to work on the project, and that too in complete isolation. He was allowed to work only after all his colleagues had left for the day, and his laboratory and freezers were fit with biometric access restrictions.
Tumpey was to wear a specialised respirator mask that allowed him to breathe only filtered air. He was required to wear two pairs of gloves, shoe covers, and a full-body surgical gown, and he would have to take a shower every time he left the laboratory. He also had to constantly take antiviral medication, and he was informed that should he contract the virus, he would be isolated and would not be able to contact anyone in the outside world, including his family.
Lung damage
Working this way, Tumpey first generated ‘recombinant’ viruses. These are artificial viruses generated in the laboratory such that they contained just the H1 and N1 gene segments from the 1918 strain, while the remaining pieces of the genetic material came from a regular laboratory strain that did not cause severe disease (in mice). The objective of his experiment was to identify which of the eight gene segments of the 1918 virus was responsible for its unprecedented power.
Tumpey thought that, when complemented with the genes from the 1918 strain, the laboratory strain might be able to cause slightly more severe disease in mice. He was wrong: the H1 and N1 genes of the 1918 virus made the laboratory strain so virulent that within five days, all the infected mice had died.
An autopsy of the deceased rodents revealed that while there was extensive lung damage, the virus was not found in the other major organs of their bodies – brain, liver, spleen, etc. The virus mainly infected the lungs, and laid waste to them.
Tumpey continued his experiments with the recombinant viruses. He found that while all eight pieces of the virus’s genetic material caused severe disease, two in particular stood out: the haemagglutinin and the RNA polymerase genes.
Suggestive, not conclusive
Haemagglutinin is the protein on the outer surface of the virus that docks with proteins on the cells of another organism. This way, the virus has a portal through to begin its invasion. The haemagglutinin segment of the 1918 strain contained modifications such that the virus could easily gain access to cells.
The viral RNA polymerase, on the other hand, makes copies of the viral genetic material. In the H1N1 strain, the polymerase was extremely efficient at this process, allowing the virus to make numerous copies of itself in a very short span of time. This then took a heavy toll on the infected cell, since the virus hijacked the cellular machinery to replicate itself.
All the experiments that Tumpey had conducted until then were suggestive, not conclusive. He had inserted pieces of the 1918 H1N1 virus inside a regular laboratory strain and found that doing so increased the virulence of the laboratory strain. Results obtained with such an experimental system would always leave room for doubt as to whether the real, complete virus would have behaved similarly. But there could be no room for doubt in this endeavour.
As a result, Tumpey had to recreate the full 1918 H1N1 influenza virus to solve this conundrum. He mixed the genetic material of all the eight individual pieces of the virus and put them in the same cell. In a few weeks, the world’s deadliest virus appeared in his cell-culture plates, back from extinction after nearly a century.
Unrivalled
The full virus demonstrated a pathogenicity unrivalled by any other influenza virus scientists have ever studied – recombinant or natural. It was highly virulent: there were 39,000-times more virions (virus particles) in the lungs of the mice infected with the 1918 virus than those infected by the more benign laboratory strain. The former lungs were filled with fluid within days, causing extensive lung damage and resulting in death.
Tumpey also found that while the haemagglutinin and the RNA polymerase genes were important reasons for the extreme nature of the 1918 virus, by themselves they did not wreak just as much havoc as when they did in combination with the other gene segments.
This is because individual genes of a virus seldom undergo changes in isolation. Every change will, likelier than not, influence other genes of the virus – especially changes that produce effects as large as those of the haemagglutinin and the polymerase genes of the 1918 virus.
All viruses have to ensure they will be transmitted to more hosts. A virus that kills its host too soon will fail at this objective because a virus is only alive as long as it is inside a host. So a change in a virus that makes it more pathogenic will either kill the host faster or it will become an easier target for the host’s immune system. Both outcomes are detrimental to the virus’s long-term survival.
So such genetic changes must be associated with alterations elsewhere in the genome that mitigate those effects on the creature’s long-term survival prospects. It could be a mutation that enhances its transmission rate, one that slows the viral life cycle, or something else that allows the virus to escape the immune system long enough for it to be transmitted.
The 1918 virus had an enhanced transmission rate due to its unique haemagglutinin, a highly active polymerase to speed up the viral replication, and (as a result) disease progression, plus a few smaller changes that allowed it to better escape the immune system. Taken together, it had the perfect tools in its arsenal to make it the ultimate killing machine.
A new benchmark
The work of Jeffery Taubenberger, Ann Reid, Johan Hultin (described in the previous article), Terrence Tumpey, and other scientists who were involved in the effort collectively showed to the world how the 1918 influenza virus originated, and why it was so deadly. Taubenberger and Reid’s determination of the genetic sequence also laid the foundation for future scientists to better understand how the influenza virus causes disease.
More importantly, their work created a benchmark. The 1918 H1N1 strain was the deadliest influenza virus to ever strike humans. By thoroughly characterising its genetic features, the researchers set the stage for others to discern similar features in the various influenza variants circulating today, which in turn eased the way to better vaccine designs, with higher efficacy, as well as to other therapeutics to prevent the disease from emerging as a global health concern once more.
Since 1918, there have been three major influenza pandemics: in 1957, 1968, and 2009. None of them were as severe as the one in 1918. The death tolls in 1957 and 1968 were estimated at 1 million; that in 2009 was lower, around 0.3 million.
But the 1918 influenza pandemic is a reminder to us all, especially in the wake of the COVID-19 pandemic, that ever so rarely, nature will arrive at that perfect, deadly combination after mixing thousands of genes and end up creating something as destructive as the 1918 H1N1 influenza virus. Ironically, nature’s ability to do so is at the very heart of evolution, and of all life on earth.
Arun Panchapakesan is an assistant professor at the Y.R. Gaithonde Centre for AIDS Research and Education, Chennai.