
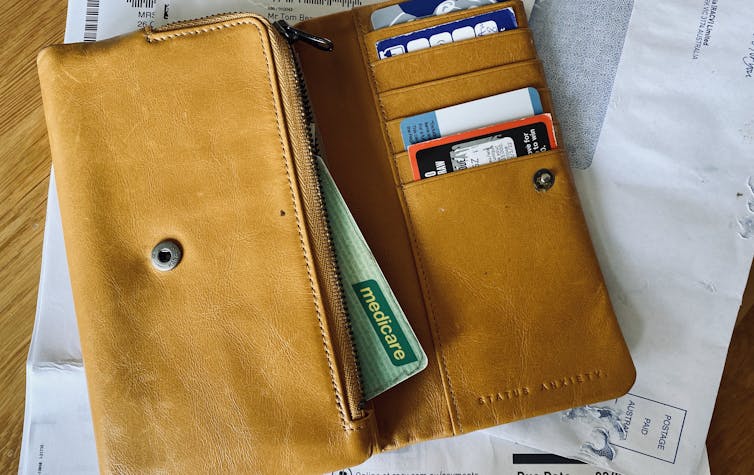
GPs have been sounding the alarm over rising costs of providing care – compounded by the pandemic and more complex demands. Many have said they are abandoning bulk billing, the Medicare scheme that pays doctors a flat rate for providing consultations.
GPs earn considerably less than other medical specialists, sometimes two or three times less annually. If GPs maintain high rates of bulk billing and the Medicare repayment rate doesn’t cover their costs, practices become unsustainable.
Health-care quality can also decline, as GPs try to see more patients in a day to clock more bulk-billing fees. But opting out of bulk billing, as our specialist colleagues have done, could mean some patients lose access to care.
Meanwhile, more than 13% of voters who responded to The Conversation’s #SetTheAgenda poll were worried about health. Cost-of-living pressures were also on their list of concerns before the election.
The Australian Medical Association (AMA) has long supported GPs moving away from bulk billing so they don’t have to depend on government to set their incomes. This time around, many GPs will heed the call, and leave patients with a larger gap fee to pay. Here’s why.
Read more: Explainer: what is Medicare and how does it work?
The rising cost of health care
General medical practices are essentially small, private businesses, which are free to set their own fees and working conditions. Medicare is a government insurance scheme to help patients access private GPs.
Medicare Benefits Schedule (MBS) fees are raised each year in accordance with the government’s Wage Price Index. This approach has long been criticised for failing to keep pace with inflation in the health sector.
Compounding this lag, rebates were frozen in 2013 as a cost-cutting measure for attendance items until July 2018.
Total spending on health in 2021–22 is estimated to be A$98.3 billion, representing 16.7% of the federal government’s total expenditure. Around 6.5% of total health expenditure is allocated to delivering GP services.
The gap between the AMA-recommended fee (around $86) and the Medicare rebate for a standard GP consult ($39.10) has grown by $13.50 over a decade to around $47. Average patient out-of-pocket costs for services directly provided by GPs have increased by 50% over the last decade.
Some 88.4% of GP services were bulk-billed in the final quarter of 2021, an increase of 0.3% on the previous year, according to the Department of Health. But much of this increase can be explained by mandated bulk-billed telehealth consultations under COVID rules, which replaced in-person consultations during lockdowns. The percentage of bulk-billed consultations was also down on the previous quarter.
Health care consumer confidence
So, health care costs in Australia are rising faster than cost of living pressures and wages growth. And there is ample evidence out-of-pocket costs create barriers to people getting health care – especially for many who need it most: rural populations, young families, those with disabilities and chronic conditions.
Earlier this year, a large survey found 30% of people with chronic conditions were not confident they could afford health care if they became seriously ill; 14% of people with chronic conditions said they could not afford healthcare or medicine now.
Rising out-of-pocket costs for health care is an important issue the major parties have not yet substantially addressed during the election campaign. The Labor party has finally come to the table with a funding promise to better support GPs and primary care, which the AMA has applauded as a good start.
Read more: How do the major parties rate on Medicare? We asked 5 experts
GPs feeling the strain
General practices have worked hard to adapt to funding squeezes by creating efficiencies of scale (boosting practice size); adopting new technology, and seeing more patients with shorter consultation times. But around half are concerned about the long-term viability of their practices.
Anecdotally, younger GPs say they are thinking about leaving face-to-face general practice, finding the demands and expectations unsustainable. Even sadder is their perception the specialty has been devalued and deskilled.
Due to the lower income and status of general practice, medical students have a limited interest in pursuing it as a career and registrar training places go unfilled.
So, the GP workforce gets older. Some 50% of GPs are now over 50. Around 80% of GPs think better pay would attract more graduates to the specialty.
The pandemic has compounded the strain on our health workforce, with GP clinics shouldering significant responsibility for testing, vaccinating and caring for COVID patients. Staff and supply shortages and inadequate funding models have put substantial stress onto an already busy and demanding career.
No quick fixes
It’s understandable that many GPs are opting out of bulk-billing. But there are no simple solutions for delivering high quality health care to everyone.
Adopting new funding models, including more blended payments – moving away from fee-for-service and incorporating “pay for performance” funding – could ease the strains on general practices.
Our health system is due for some courageous reforms. GPs have long advocated for better telehealth, reducing the current funding bias towards procedural medicine, and more consultation tiers, to improve quality of care. A strong Medicare system is important to provide a safety net, ensuring equitable access for all Australians.
David King does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
This article was originally published on The Conversation. Read the original article.







