As bird flu spreads among dairy cattle in the U.S., veterinarians and researchers have taken note of Finland’s move to vaccinate farmworkers at risk of infection. They wonder why their government doesn’t do the same.
“Farmworkers, veterinarians, and producers are handling large volumes of milk that can contain high levels of bird flu virus,” said Kay Russo, a livestock and poultry veterinarian in Fort Collins, Colorado. “If a vaccine seems to provide some immunity, I think it should be offered to them.”
Among a dozen virology and outbreak experts interviewed by KFF Health News, most agree with Russo. They said people who work with dairy cows should be offered vaccination for a disease that has killed roughly half of the people known to have gotten it globally over the past two decades, has killed cats in the U.S. this year, and has pandemic potential.
However, some researchers sided with the Centers for Disease Control and Prevention in recommending against vaccination for now. There’s no evidence that this year’s bird flu virus spreads between people or causes serious disease in humans. And it’s unclear how well the available vaccine would prevent either scenario.
But the wait-and-see approach “is a gamble,” said Jennifer Nuzzo, director of the Pandemic Center at Brown University. “By the time we see severe outcomes, it means a lot of people have been infected.”
“Now is the time to offer the vaccines to farmworkers in the United States,” said Nahid Bhadelia, director of the Boston University Center on Emerging Infectious Diseases. Even more urgent measures are lagging in the U.S., she added. Testing of farmworkers and cows is sorely needed to detect the H5N1 bird flu virus, study it, and extinguish it before it becomes a fixture on farms — posing an ever-present pandemic threat.
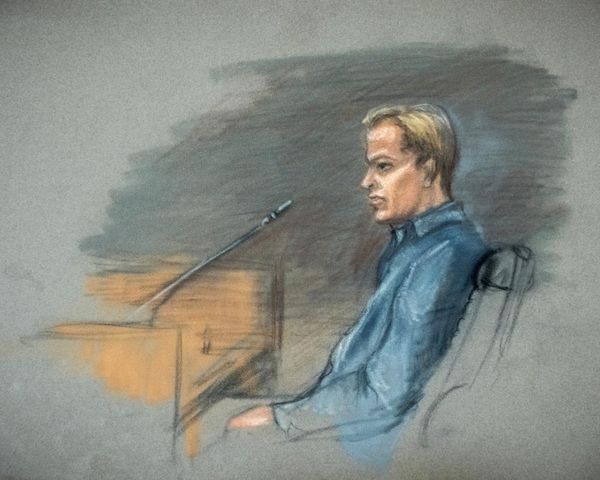
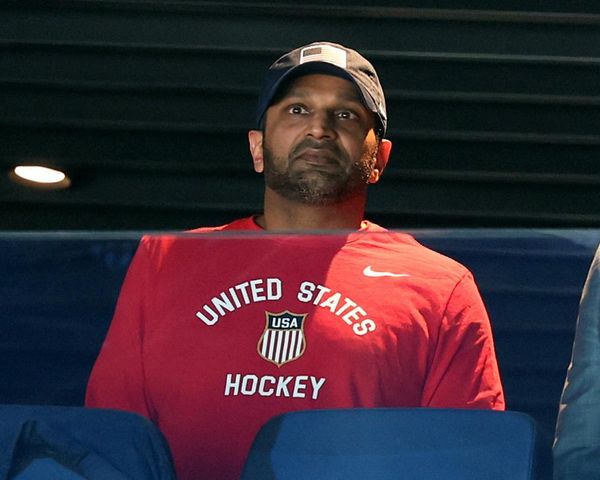
Demetre Daskalakis, director of the CDC’s National Center for Immunization and Respiratory Diseases, said the agency takes bird flu seriously, and the U.S. is stockpiling 4.8 million doses of the vaccine. But, he said, “there’s no recommendation to launch a vaccine campaign.”
“It’s all about risk-benefit ratios,” Daskalakis said. The benefits are blurry because there hasn’t been enough testing to understand how easily the virus jumps from cows into people, and how sick they become. Just four people in the United States have tested positive this year, with mild cases — too few to draw conclusions.
Other farmworkers and veterinarians working on dairy farms with outbreaks have reported being sick, Russo said, but they haven’t been tested. Public health labs have tested only about 50 people for the bird flu since the outbreak was detected in March.
Still, Daskalakis said the CDC is not concerned that the agency is missing worrisome bird flu infections because of its influenza surveillance system. Hospitals report patients with severe cases of flu, and numbers are normal this year.
Another signal that puts the agency at ease is that the virus doesn’t yet have mutations that allow it to spread rapidly between people as they sneeze and breathe. “If we start to see changes in the virus, that’s another factor that would be part of the decision to move from a planning phase into an operational one,” Daskalakis said.
On July 8, researchers reported that the virus may be closer to spreading between people than previously thought. It still doesn’t appear to do so, but experiments suggest it has the ability to infect human airways. It also spread between two laboratory ferrets through the air.
In considering vaccines, the agency takes a cue from a 1976 outbreak of the swine flu. Officials initially feared a repeat of the 1918 swine flu pandemic that killed roughly half a million people in the United States. So they rapidly vaccinated nearly 43 million people in the country within a year.
But swine flu cases turned out to be mild that year. This made the vaccine seem unnecessarily risky as several reports of a potentially deadly disorder, Guillain-Barré Syndrome, emerged. Roughly one of every million people who get influenza vaccines may acquire the disorder, according to the CDC. That risk is outweighed by the benefits of prevention. Since Oct. 1, as many as 830,000 people have been hospitalized for the seasonal flu and 25,000 to 75,000 people have died.
An after-action report on the 1976 swine flu situation called it a “sobering, cautionary tale” about responding prematurely to an uncertain public health threat. “It’s a story about what happens when you launch a vaccine program where you are accepting risk without any benefit,” Daskalakis said.
Paul Offit, a virologist at the Children’s Hospital of Philadelphia, sides with the CDC. “I’d wait for more data,” he said.
However, other researchers say this isn’t comparable to 1976 because they aren’t suggesting that the U.S. vaccinate tens of millions of people. Rather they’re talking about a voluntary vaccine for thousands of people in close contact with livestock. This lessens the chance of rare adverse effects.
The bird flu vaccine on hand, made by the flu vaccine company CSL Seqirus, was authorized last year by the European equivalent of the FDA. An older variety has FDA approval, but the newer variety hasn’t gotten the green light yet.
Although the vaccine targets a different bird flu strain than the H5N1 virus now circulating in cows, studies show it triggers an immune response against both varieties. It’s considered safe because it uses the same egg-based vaccine technology deployed every year in seasonal flu vaccines.
For these reasons, the United States, the United Kingdom, the Netherlands, and about a dozen other countries are stockpiling millions of doses. Finland expects to offer them to people who work on fur farms this month as a precaution because its mink and fox farms were hit by the bird flu last year.
In contrast, mRNA vaccines being developed against the bird flu would be a first for influenza. On July 2, the U.S. government announced that it would pay Moderna $176 million for their development, and that the vaccines may enter clinical trials next year. Used widely against covid-19, this newer technology uses mRNA to teach the immune system how to recognize particular viruses.
In the meantime, Florian Krammer, a flu virologist at Mount Sinai’s Icahn School of Medicine, said people who work on dairy farms should have the option to get the egg-based vaccine. It elicits an immune response against a primary component of the H5N1 bird flu virus that should confer a degree of protection against infection and serious sickness, he said.
Still, its protection wouldn’t be 100%. And no one knows how many cases and hospitalizations it would prevent since it hasn’t been used to combat this year’s virus. Such data should be collected in studies that track the outcomes of people who opt to get one, he said.
Krammer isn’t assuaged by the lack of severe bird flu cases spotted in clinics. “If you see a signal in hospitals, the cat is out of the bag. Game over, we have a pandemic,” he said. “That’s what we want to avoid.”
He and others stressed that the United States should be doing everything it can to curb infections before flu season starts in October. The vaccine could provide an additional layer of protection on top of testing, wearing gloves, and goggles, and disinfecting milking equipment. Scientists worry that if people get the bird flu and the seasonal flu simultaneously, bird flu viruses could snag adaptations from seasonal viruses that allow them to spread swiftly among humans.
They also note it could take months to distribute the vaccines after they’re recommended since it requires outreach. People who work beside dairy cows still lack information on the virus, four months into this outbreak, said Bethany Boggess Alcauter, director of research at the National Center for Farmworker Health.
Health officials have talked with dairy farm owners, but Boggess’ interviews with farmworkers suggest those conversations haven’t trickled down to their staff. One farmworker in the Texas Panhandle told her he was directed to disinfect his hands and boots to protect cows from diseases that workers may carry. “They never told us if the cow could infect us with some illness,” the farmworker said in Spanish.
The slow pace of educational outreach is a reminder that everything takes time, including vaccine decisions. When deciding whether to recommend vaccines, the CDC typically seeks guidance from its Advisory Committee on Immunization Practices, or the ACIP. A consultant to the group, infectious disease researcher William Schaffner, has repeatedly asked the agency to present its thinking on Seqirus’ bird flu vaccine.
Rather than fret about the 1976 swine flu situation, Schaffner suggested the CDC consider the 2009-10 swine flu pandemic. It caused more than 274,000 hospitalizations and 12,000 deaths in the U.S. within a year. By the time vaccines were rolled out, he said, much of the damage had been done.
“The time to discuss this with ACIP is now,” said Schaffner, before the bird flu becomes a public health emergency. “We don’t want to discuss this until the cows come home in the middle of a crisis.”
Subscribe to KFF Health News' free Morning Briefing.