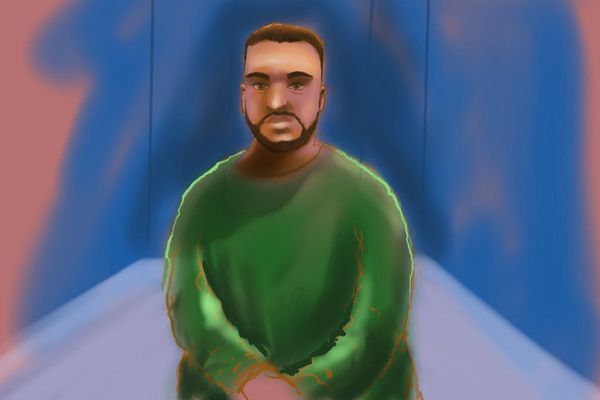
Selina and Rhonda Bob are waiting for a lifesaving phone call — one that could be years away.
Their kidneys are failing, and they hope they won't have to wait too long on the organ transplant list.
"I was feeling sad when I heard the doctors say to me you're going to be in renal [failure] soon. I thought, 'you must be lying'," Selina said.
Every week, the sisters are bound to a chair for 16 hours as their blood is pumped out of their bodies and filtered through a dialysis machine.
The pair were both diagnosed with diabetes – a disease that can damage the kidneys — at a staggeringly young age.
And in this isolated pocket of the world, these sisters are not alone in their prognosis.
New research has found that rates of diabetes in Central Australia are amongst the highest ever seen worldwide – and they are getting worse, with more people diagnosed every year at far younger ages than ever seen before.
The study, published in the open access medical journal BMJ Open, analysed seven years' worth of health data from more than 21,000 Aboriginal people from 51 remote communities across the Northern Territory.
The lead author is Matthew Hare, an endocrinologist at Royal Darwin Hospital and senior research officer at Menzies School of Health Research.
He said the new research showed a growing diabetes epidemic in remote NT communities, which was "unprecedented in terms of prevalence".
"Rates of diabetes in these remote communities are increasing such that now 29 per cent of adults in remote Aboriginal communities are living with diabetes, and this is largely type 2 diabetes," Dr Hare said.
"The findings of our research were particularly concerning for the Central Australian region where communities are having diabetes prevalence rates up to 40 per cent of adults."
Dr Hare said the last time this type of research was conducted was in 2012, and things had gotten much worse since then.
Diabetes no longer a disease of the elderly
Up until now, diabetes was thought to be a disease that mainly affected older people, but Dr Hare said type 2 diabetes was being seen increasingly in children.
"We have seen cases diagnosed as young as age four," Dr Hare said.
"And that's type 2 diabetes, which we previously thought was a condition mostly seen in adults.
"We are seeing the average age of diagnosis of type 2 diabetes being in the mid-30s, which compared to national data is decades younger.
"When you look at the Australian population, nationally, most people getting diagnosed with type 2 diabetes are in their 60s or 70s."
Co-author Dr Amy Rosser, a senior remote medical practitioner in a desert community about 300km from Alice Springs, said Aboriginal people aged 20-39 years in remote parts of the NT were 26 times more likely to be diagnosed with type 2 diabetes than people of the same age in the national Australian population.
Epidemic related to impacts of colonisation
Dr Hare said there were numerous drivers behind the growing epidemic, including the intergenerational effects of diabetes in pregnancy and the social and economic disparities still experienced by many people in remote communities today.
"But really, we think this epidemic is largely grounded in the impacts of colonisation and the dramatic changes in ways of life that has caused for many people living in remote Aboriginal communities," he said.
Selina and Rhonda Bob said diabetes was in the "family line".
"[Our mother] went through renal," Selina said.
"We found out we are diabetic when we were young … I found out when I was 18 years old."
It meant the pair were eventually forced to leave their home and family, as their community of Areyonga, like many remote places in the NT, didn't provide access to dialysis treatment.
Urgent need for prevention strategies
The top doctor at one of Central Australia's key Aboriginal health bodies, Dr John Boffa, said he rarely saw diabetes in his patients in the late 80s.
But these days, his big challenge is trying to close the life expectancy gap caused by preventable chronic diseases.
While the statistics seem dire, the chief medical officer at Central Australian Aboriginal Congress said there was some good news.
"Diabetes is a potentially reversible condition," he said.
"And there are significant numbers of Aboriginal people who have completely reversed their diabetes, got off all their medications, by losing weight."
He said low-calorie diets and bariatric surgery were the main ways people in Central Australia were losing weight, despite the hefty price tag of the surgery.
"Some of those people are paying close to $30,000 to access that surgery, and they are using superannuation and other funds to do that because the waiting time in public hospitals is extremely long," Dr Boffa said.
Dr Hare said while the government was pouring a lot of funding and resources into the treatment of diabetes it was time to invest in prevention strategies in partnership with Aboriginal community members.
"We need to be improving access to fresh, quality, nutritious food, and addressing the issues with education and employment [and] overcrowded housing that are all social determinants of chronic conditions such as diabetes," he said.
The Bob sisters are living proof that a healthy lifestyle goes a long way toward managing diabetes.
Every week the pair dance, punch and lift the sugar away in exercise classes at the Purple House, an Indigenous-owned and run health service operating in Alice Springs, and they've never felt better.
And while the workouts won't repair their kidneys, movement and healthy eating could reverse their diabetes.