
Last year, the sheriff of San Diego County shared “traumatic” footage of one of his deputies collapsing after handling a white powder. Officers administered four doses of the overdose-reversing medication naloxone. His training officer said the deputy was “OD’ing the whole way to the hospital.”
Sheriff Bill Gore told The San Diego Tribune that the officer experienced “classic signs of fentanyl overdose” but was “shocked” that medical experts determined that what the officer went through was definitely not that.
In 2017, a local television news outlet in Ohio reported that an officer “passed out at the station from overdosing on the white powder that police think was fentanyl” that he “brushed” from his shirt during a traffic stop. The following year, the man arrested during the stop was sentenced to six-and-a-half years in prison for charges that included assaulting that officer.
None of what these officers experienced was an overdose, based on multiple assessments from toxicologists, public health experts, drug policy researchers and law enforcement agencies’ own guidance when it comes to fentanyl.
Dozens of police reports of officers experiencing secondhand fentanyl overdoses over the last several years after some form of exposure are largely the same. They allegedly come into contact with a substance through the skin or in the air, they feel lightheaded or dizzy, they pass out. Their heart races. Chest tightens. None of these are symptoms of an opioid overdose.
But local and national news outlets and social media posts are amplifying officers’ warnings of the dangers of the synthetic opioid as a growing threat to their own jobs – what analysts fear is being used to help fund their latest front in the war on drugs, keep people in jail, and criminalise life-saving treatment.
The spread of viral fentanyl misinformation reflects a complex phenomenon – from news outlets’ deferential relationships with law enforcement agencies, to the ways in which police fuel public perceptions of the risks associated with the job, used to bolster demands for larger budgets and increase criminal penalties.
These reports also lack critical information or public health guidance about how to combat a crisis that has impacted thousands of people and their friends and families, with stories of people who use drugs – people who have relied on life-saving treatment after an actual overdose – often missing from that coverage.
In Kansas City, Kansas, emergency responders reported using five rounds of naloxone on an officer who allegedly found pills on a person in custody. After collapsing on the ground, video shows the officer gasping for air while other officers, panicking, repeatedly spray the medication up his nose.
A local news outlet was roundly criticised for its story (“‘I knew I was dying’: How 5 rounds of Narcan possibly saved KCK police officer’s life”), then issued a clarification to stand by its reporting, noting that the network “reached out” to the US Drug Enforcement Agency.
“It’s like that Spider-Man where they’re all pointing at one another,” says Dr Ryan McNeil, director of Harm Reduction Research at Yale School of Medicine’s Program in Addiction Medicine.
“What do these stories do? They reinforce the impression for so many people that fentanyl is the equivalent of some kind of magical weapon of mass destruction floating around out there that if one happens to be in the presence of, they’re in immediate danger,” he tells The Independent.
This month, the attorney general of Florida called on President Joe Biden to call it just that, pointing to a wave of overdoses in the state, including a first responder at the scene of an overdose.
“If we think about this as something that is seen as increasing the ‘potential’ risk to police, it serves as a justification for the further militarization of the police and dehumanization of people who use drugs,” Dr McNeil says. “Within a broader context of people not trusting the media, this is a perfect example of, you know, in some cases, maybe they shouldn’t.”
‘This wouldn’t be chemically or physically possible, at all’
More than 107,000 Americans died from drug overdoses in the year between September 2020 and September 2021, according to the US Centers for Disease Control and Prevention. In September 2015, roughly 52,000 people died from overdoses in a similar timeframe.
That surge in drug-related deaths accelerated with the proliferation of the powerful synthetic opioid fentanyl. Nearly two-thirds of all overdose deaths reported within that time involved synthetic opioids, including according to federal data, and many were preventable.
Fentanyl is currently legal to treat patients with severe pain and is commonly used for pain management under doctor supervision. It is far more potent than heroin, which can heighten the risk of an overdose. But its proliferation largely follows heightened demand for heroin, with illicitly manufactured fentanyl “cut” into drug supplies, often without people who use drugs realising what they are using.
Signs of an overdose include shallow breathing, loss of consciousness, and pale and ashen or clammy skin.
It is not possible to overdose from fentanyl through accidental skin contact or from being in close proximity to the drug, according to Dr Ryan Marino, a medical toxicologist with Case Western Reserve University School of Medicine. The only way to overdose from fentanyl is through injecting or ingesting it in some way, or through transdermal fentanyl patches in large quantities over long periods of time.
The American College of Medical Toxicology and the American Academy of Clinical Toxicology also issued a joint statement in 2017 concluding that “incidental dermal absorption is very unlikely to cause opioid toxicity” and that “toxicity cannot occur from simply being in proximity to the drug.”
Ryan Feldman, a clinical toxicologist and emergency-medicine pharmacist, also co-published a case study about an accident in which he spilled a large amount of liquid fentanyl all over himself while at work. He washed it off, with “no clinical effects of opioid exposure observed.”
One report from the US Centers for Disease Control and Prevention, following a field study, found that investigators were “definitively” unable to figure out how police were experiencing the symptoms they reported.
“Fentanyl just doesn’t absorb through the skin and doesn’t just get into the air. And this wouldn’t be chemically or physically possible, at all,” Dr Marino tells The Independent.
Dr Marino was among dozens of health experts and drug researchers who issued an open letter to news outlets and law enforcement agencies demanding they retract “dangerous drug misinformation” about fentanyl use and overdoses.
“The reason I care so much about this myth and many others do is because there are real consequences and real harms that happen from it,” Dr Marino tells The Independent. “And we talk a lot about how this leads to delays in care of people who are overdosing and it leads to the further stigma of people who use drugs, it leads to increased criminalization.”
A 2021 study published by the Health & Justice journal found that, among a group of police officers, nearly 80 per cent believed they were at “great risk of overdose” from touching or inhaling fentanyl. But after a training programme, more than 60 per cent disagreed with the same statement.
“Misinformation about overdose risk from accidentally inhaling or touching fentanyl is widespread among police,” according to the report. “This may aggravate already elevated burdens of officer stress and burnout, while chilling lifesaving overdose response. Police education has shown promise in reducing false beliefs about fentanyl.”
Toxicologists believe it is more likely that police – believing guidance that being exposed to fentanyl could lead to a fatal overdose – may be experiencing panic attacks or the result of a so-called “nocebo” effect.
“Where a placebo works, if you believe something is going to help … you can have kind of beneficial symptoms or improvement from it. And the flipside is true, where if you believe so much that something is so deadly it’s going to hurt you so bad,” Dr Marino says. “If you think fentanyl kills you from touching it, and then you think you touched fentanyl, you’re going to experience very real symptoms from that.”
A new frontier in the war on drugs
Nancy Chartrand, a media relations specialist with the Kansas City Police Department, tells The Independent that the agency is “constantly messaging to the community the dangers of fentanyl,” including through partnerships with local school districts and in community town hall meetings.
The alleged accidental overdose of one of the department’s officers has “heightened” the urgency around the issue, she says.
Law enforcement agencies like the Kansas City Police Department routinely rely on the US Drug Enforcement Agency’s guidance on fentanyl exposure and handling.
When asked for teaching materials, best practices or guidance around recognising signs of opioid overdoses that the agency shares with local law enforcement, a spokesperson for the federal agency directed The Independent to the US Centers for Disease Control and Prevention.
The DEA “follows the CDC’s guidelines for preventing occupational exposure to fentanyl,” according to DEA spokesperson Katherine Pfaff.
CDC spokesperson Scott Paul said that skin contact fentanyl exposure “is not likely to lead to an overdose unless large volumes of highly concentrated powder are encountered over a long period of time.”
“Brief skin contact with powdered fentanyl or its analogues is not expected to lead to toxic effects if any visible contamination is promptly removed using soap and water,” he said in a statement to The Independent
“The potential ways people come into contact with fentanyl and its analogues of greatest concern include breathing it in, contact with mucous membranes such as the eyes, ears, inside the nose, or inside the mouth, by eating, drinking, and swallowing, and skin puncture (e.g., needlestick),” he added. “Any of these exposure routes can potentially result in a variety of symptoms that can include the rapid onset of life-threatening respiratory depression, or slowed breathing.”
That guidance follows now-removed instruction from the DEA given to law enforcemement agencies in 2016, claiming that “fentanyl can be absorbed through the skin or accidental inhalation of airborne powder can also occur” and that “just touching fentanyl or accidentally inhaling the substance during enforcement activity or field testing the substance can result in absorption through the skin” with the “onset of adverse health effects, such as disorientation, coughing, sedation, respiratory distress or cardiac arrest” coming on “very rapid and profound” and “within minutes of exposure.”
Over the last several decades, alongside a growing local news focus on crime, local law enforcement agencies across the US grew increasingly militarised, while the cities they served were depicted as lawless havens for people who use drugs and the criminal enterprises that exploited them.
But the scope of the overdose crisis has exploded beyond the narrow and often racist drug war coverage that has dominated local news, with more than 3,000 Americans dying every week.

Drug policy experts and analysts suggest the spread of fentanyl misinformation is used to reinforce law enforcement’s demands for increasingly larger budgets, while justifying severe criminal penalties in the latest front on the war on drugs.
Despite an increase in overdose deaths, several states have criminalised fentanyl test strips, inexpensive strips that can be used to identify the presence of fentanyl in drugs. A growing number of states have made them easier to access, but they are considered illegal drug paraphernalia in roughly half the US.
And in cases like the one in Ohio, prosecutors across the US are charging people for crimes connected to officers reporting being exposed to fentanyl, jailing people for accidentally exposing police to a drug in a way that health experts say cannot even happen.
People who overdose also are at risk of incarceration following their interaction with emergency responders who save their lives. One study among EMS calls in Indianapolis, Indiana from 2019 through 2020 found that one in every 10 overdose incidents resulted in an arrest.
“We are in the midst of a record number of overdose deaths due to opioids, and at the same time, there is propaganda and stigma and a lot of unfounded fear around fentanyl and fentanyl analogs,” according to Maritza Perez, director of the office of federal affairs at the Drug Policy Alliance.
“Obviously, fentanyl analogs can cause harm, and people should be empowered to recognize that harm,” she tells The Independent. “But certainly bad science and false facts about fentanyl and fentanyl analogs are not helpful. … My biggest fear is that it will create even more stigma, and will disencourage people from helping people when they’re experiencing an overdose … or fear for themselves overdosing or because there will be [risk] of being criminalized for it.”
How overdose stories explode on social media
A woman was hospitalised after “touching” a dollar bill in Tennessee that she believed contained fentanyl. She told local news outlets – airing images of the woman in a hospital bed, staring blankly – that she went “numb” minutes later and she could barely talk or breathe before passing out.
The story was shared in national news outlets; The New York Post ran a headline reading “I picked up a dollar on the ground – and nearly died.” The Metropolitan Nashville Police Department did not find any evidence of fentanyl.
That story follows other reports across the US about police reportedly finding evidence of fentanyl on dollar bills. Similarly dubious viral claims were rampant in 2017 over warnings that people were leaving traces of fentanyl on shopping cart handles.
One 2020 study found that media reports containing fentanyl misinformation were shared roughly 450,000 times on Facebook, reaching nearly 70 million people between 2015 and 2019. Corrections or attempts to debunk false claims about fentanyl reached only 4.6 million people through fewer than 30,000 shares.

The spread of spurious claims of officers overdosing from fentanyl also points to the relationship that local law enforcement agencies have with news media, and the lack of scrutiny applied to police statements regarded as fact.
“A big part of this idea that fentanyl is some sort of big scary boogeyman comes from the repeated coverage of fentanyl, the fentanyl crisis, fentanyl overdoses, fentanyl deaths – those are things that should be covered that people do need to know about, but at this point to not have any kind of knowledge of fentanyl, while reporting on fentanyl, is a big public disservice,” Dr Marino tells The Independent.
“If there’s this deference to police authority that’s proven to consistently be wrong, then maybe we need to rethink that in reporting,” according to Dr McNeil. “Because the flip side of this is it just seems symptomatic of that much larger tendency among American journalists to refer to police as if it’s gospel. And these stories are the perfect example of the type of thing that doesn’t hold up to scrutiny.”
There is a wealth of drug information available across federal public health agencies and among drug researchers, published in science journals and readily available elsewhere. But even as more news outlets debunk false narratives around fentanyl exposure, reports of police officers allegedly overdosing from accidental contact persist.
On 20 July, a sheriff’s deputy in Richland County, South Carolina reported losing consciousness and was administered naloxone after patting down a person in custody. The deputy did not report seeing any drugs. Two days later, a Genesee County sheriff’s deputy in Minnesota fell to his knees and “blacked out” after assisting an inmate who overdosed inside Genesee County Jail. On 27 July, the sheriff of Canyon County, Idaho told Fox News that “numerous” deputies have been hospitalised for fentanyl exposure.
“Every time one of these stories comes on … it elevates those of police and the overblown, absurd, perceived risk associated with fentanyl, above the lives of people who use drugs were actually dying, day in and day out,” according to Dr McNeil. “So every time you see a story like this, it’s an expression of the fact that people who use drugs don’t really matter to them. And unfortunately, I think that’s entirely consistent with how a large portion of the population actually feels about people who use drugs. And that creates the broader context in which stories like this go viral.”
A public health failure
If law enforcement officers tell the public that approaching someone who has overdosed or a scene where drugs are present could put them in danger, “that puts people at risk,” Dr Marino tells The Independent.
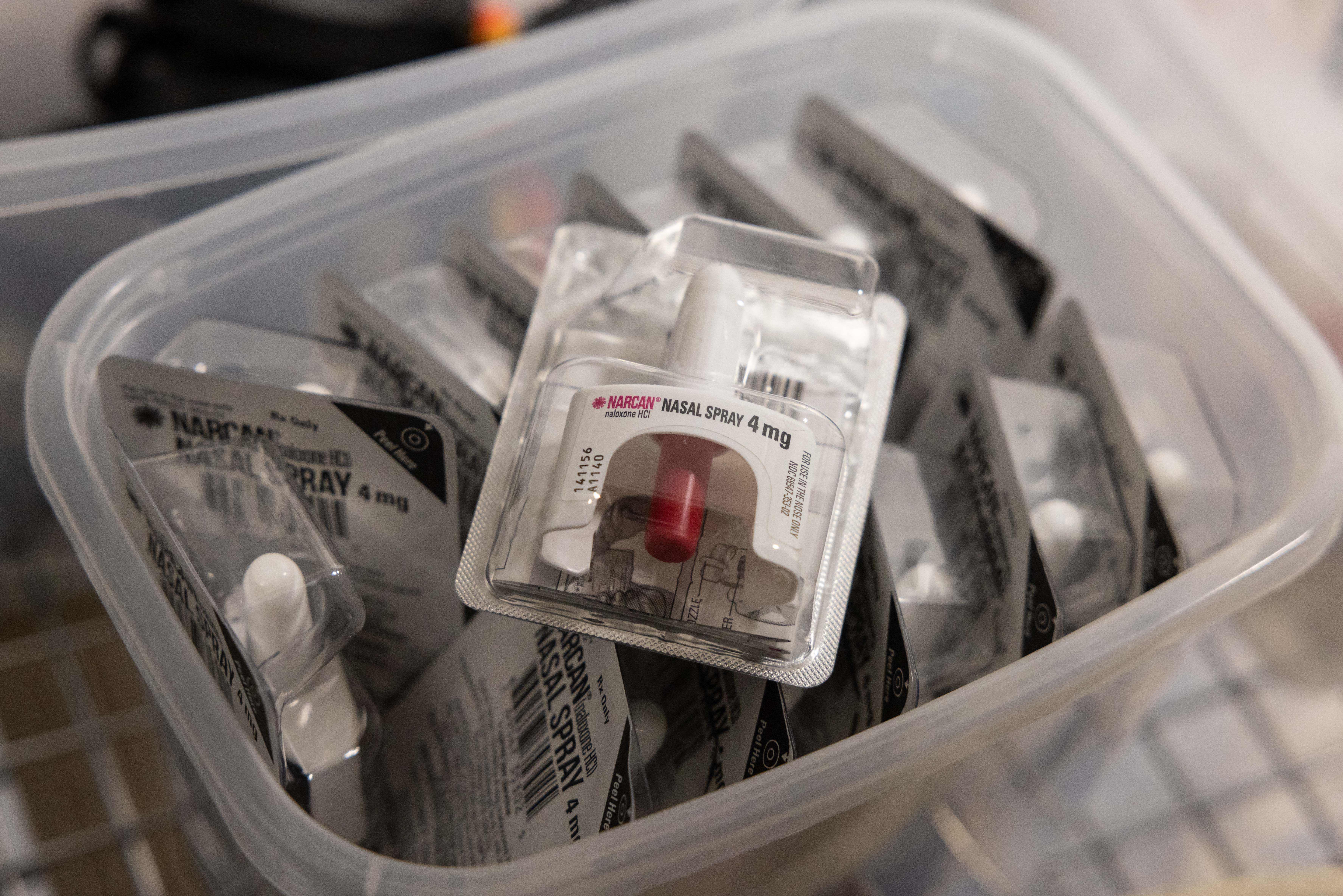
“Time is critical,” he says. “These are very easy-to-treat situations. Nobody should ever die from an opioid overdose. We have an antidote for it.”
Dr Marino contrasts public health messaging around fentanyl and opioid overdoses to the one centred around Covid-19, and the lack of approachable and readily available public messaging around a parallel crisis.
“The fact that people don’t actually know the symptoms of opioid overdose at this point in 2022 is kind of unacceptable, I think, as a society, when we have more than 100,000 people a year dying of overdoses, which are completely preventable, and completely treatable,” he says.
News outlets, then, have an obligation to tell people how to identify overdose, what to do in case a loved one is overdosing, how to access naloxone, and offer instructions for using it.
“If they covered it from that angle versus a criminal one, people would be more likely to seek help, especially if a loved one is overdosing, or if they themselves feel like they need treatment or access to health services,” Ms Perez tells The Independent. “The propaganda, the fear, the stigma will not help with that. It’s causing more pain at a time when people really need support.”







