Healthcare charities and patient groups are calling on NHS England to reintroduce Covid-19 precautions for staff, amid fears that clinically vulnerable patients and medics will be put at risk this winter.
Since Covid safety measures were dropped earlier in the year, staff in NHS England are no longer required to wear a mask in clinical settings. Most healthcare workers who have symptoms of a respiratory infection are no longer asked to test for Covid.
The number of people testing positive in England rose 30% in the seven days to 30 September, to 16,000 cases. Hospitalisations went up 25% over the same period to 3,800, according to government figures.
Charities and organisations, including Blood Cancer UK, Anthony Nolan, Kidney Care UK, Mencap, Forgotten Lives UK, and Clinically Vulnerable Families have called for patients to have the right to request a staff member wear a mask, as well as for the reintroduction of symptomatic testing in all cases. Some are also calling for asymptomatic testing for staff working near patients who at risk of becoming severely ill or dying from the virus.
Clinically vulnerable people say that they are missing vital medical care since protections in healthcare settings have been removed. Others have been seen by staff with Covid symptoms and no mask, despite saying that they were vulnerable. GP surgeries and hospitals are often high-risk settings because of the numbers of clinically vulnerable people who rely on them and the level of social mixing.
“Many of the most vulnerable are facing an impossible choice between accessing essential medical treatment and placing themselves at heightened risk of coronavirus and in the very places they should be safest,” said Mark Oakley, spokesperson for Forgotten Lives UK. “Our members tell us they are now cancelling or postponing treatments and we’re seeing this cause more health problems.” He said that there should be simple, cost-effective precautions, such as masking and regular testing, to remove this inequality of access to healthcare. “No patient should be fearful of entering a hospital, GP surgery or vaccine centre.”

A survey by Forgotten Lives UK, seen exclusively by the Observer, found that half of clinically vulnerable people surveyed had cancelled a medical appointment over concerns about lack of Covid precautions. More than a quarter had cancelled or declined a vaccine booster for the same reason.
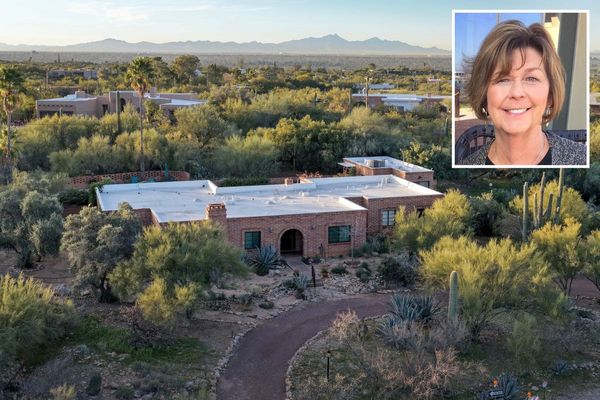
Glynis Huskisson – who is immunocompromised because of a kidney transplant and chronic obstructive pulmonary disease, and has not produced sufficient antibodies from the vaccine – has been told by her consultant to “avoid Covid at all costs”. Most of her healthcare team do not wear masks or test for the virus.
The 70-year-old needs a hip replacement and surgery for nerve damage but has postponed both due to lack of precautions. She is in constant pain. Huskisson also needs surgery for an enlarged thyroid but doesn’t feel safe going ahead. “It’s growing and starting to crush my windpipe,” she said. “I feel alone and betrayed.”
Andrew Jennings* works as a senior nurse in the NHS and is “terrified”. “We’re now told not to test ourselves and we’d have to buy our own anyway. We’re advised not to wear masks in almost all situations,” he says. “It’s exhausting.”
Jennings is immunocompromised as a result of medications he takes for multiple sclerosis and has caught Covid twice at work. He was so unwell he needed antivirals and weeks off. This month, he learned that – unlike previous vaccine rollouts – NHS staff in his trust won’t be offered a booster on-site, making it “impossible” to get time off to get their jab elsewhere.
“I feel just as unsafe at work as at the height of the pandemic,” he said. “At least then, people were testing, masking and self-isolating if they were symptomatic.” Laura Challinor, senior policy and public affairs manager at Blood Cancer UK, said that the charity would like to see increased Covid testing in clinical settings. “Earlier this year, symptomatic testing in hospitals was greatly reduced. As we go into the autumn, with Covid-19 cases rising and the uncertainty of a new variant, routine testing in healthcare settings should now be reinstated to monitor and mitigate the risk for people with weakened immune systems.”
The NHS said: “While decisions on wider mask-wearing are made locally, based on risk assessments, guidance clearly recommends staff should continue to wear face masks when treating patients with Covid-19, and that universal mask-wearing should also be considered in settings where patients are at high risk of infection due to immunosuppression.”
* Name has been changed