It’s estimated almost 1.9 million Australians have diabetes, and numbers are growing. Between 2013 and 2023, the total number of people known to be living with diabetes across the country rose by 32%.
As is the case for a range of health conditions, diabetes disproportionately affects Aboriginal and Torres Strait Islander people.
Indigenous Australians are three times more likely to be diagnosed with diabetes than non-Indigenous Australians. They are 4.4 times more likely to die from it.
Among other factors, physical activity plays an important role in the prevention and management of type 2 diabetes. But our new study, published in the Medical Journal of Australia, shows we don’t know enough about the role of physical activity in preventing and managing type 2 diabetes in First Nations people.
What is diabetes?
Diabetes is a condition where there’s too much glucose (sugar) in the blood. There are different types, but the most common is type 2 diabetes. In people with type 2 diabetes, the body becomes resistant to the effects of insulin, a hormone which regulates blood sugar levels.
Risk factors for type 2 diabetes include having a family history of diabetes, being overweight, and having high blood pressure.
The high rates of diabetes in Indigenous communities are to a large extent influenced by the social determinants of health. For example, we know food insecurity disproportionately affects Aboriginal and Torres Strait Islander people, especially in rural and remote communities. This can make it difficult to follow a healthy diet, which in turn affects overall health.
People in remote Indigenous communities also often have poorer access to educational and employment opportunities, suitable housing, and high-quality health care. All these factors can contribute to poorer health.
First Nations communities have particularly high rates of younger onset type 2 diabetes (usually defined as a diagnosis before age 40).
If diabetes is not effectively managed, it can lead to a range of complications, including long-term damage to the heart, kidneys, eyes and feet. Diabetes can affect all aspects of a person’s life, including their mental health.

Lifestyle interventions (diet and physical activity) are generally recommended as part of a treatment plan for type 2 diabetes.
We wanted to understand how physical activity interventions in particular can help Aboriginal and Torres Strait Islander people with diabetes.
Our research
As well as playing a role in diabetes prevention, there’s good evidence exercise is beneficial for people already diagnosed with type 2 diabetes.
Physical activity has been associated with lower levels of glycated haemoglobin in the blood (an index of glucose control), reduced blood lipids such as cholesterol, and weight loss. Evidence suggests a combination of aerobic and resistance exercise may be superior to either mode alone.
We reviewed studies that looked at the effects of physical activity interventions and programs in type 2 diabetes prevention and management for First Nations Australians.
We found only nine studies that investigated physical activity interventions for preventing or managing type 2 diabetes in Indigenous adults.
There was some evidence linking physical activity to better outcomes in Indigenous Australians with type 2 diabetes. However, the value of the findings was affected by shortcomings in study design and a lack of involvement of Indigenous people in designing and carrying out the research.

A gap in high-quality evidence
There are many aspects of diabetes prevention and management that tend to be more difficult for people in First Nations communities, particularly those that are rural or remote.
Also, new technologies that can help with diabetes management, such as continuous glucose monitors, are often very expensive.
It’s crucial Indigenous Australians with diabetes have access to appropriate diabetes support, education and services.
Notably, health, cultural and socioeconomic disparities can impact participation in physical activity. What constitutes realistic opportunities to exercise can differ for Aboriginal and Torres Strait Islander people compared to other Australians.
Previous data has shown Indigenous Australians are less likely to meet physical activity recommendations than non-Indigenous Australians.
Factors that might influence the uptake of physical activity among First Nations people include access to safe, accessible, family-friendly and inexpensive locations to do exercise. These can be limited in regional and remote communities.
Read more: How a culturally informed model of care helped First Nations patients with heart disease
Overall, we found a lack of reliable data on whether exercise, and what type of exercise, might benefit Aboriginal and Torres Strait Islander people with type 2 diabetes.
Given physical activity is a cornerstone in the management of type 2 diabetes, we need more rigorous research in this area. These studies must be well designed and culturally appropriate. They must involve Aboriginal and Torres Strait Islander people at all levels of the research process.
Targeted research will help us determine the best approaches to increase physical activity, and understand its benefits, for Indigenous people with type 2 diabetes.
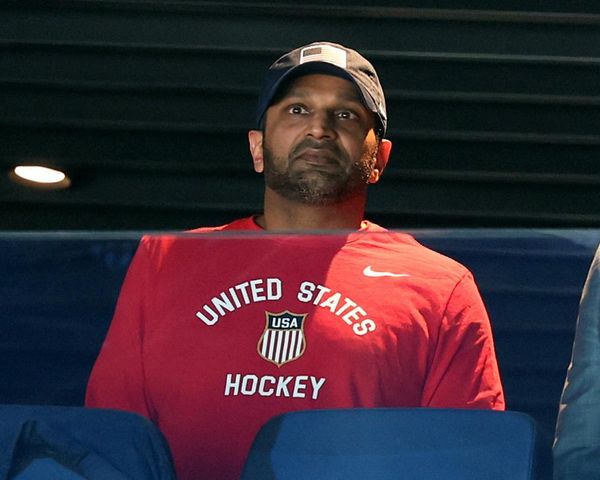
Ray Kelly is a Director at Ray Kelly Fitness Pty Ltd, which provides lifestyle programs in partnership with Aboriginal medical services. He has received funding from Primary Health Networks, the NSW Ministry of Health, and directly from Aboriginal medical services. Ray has also received MRFF funding for his research.
Margaret Morris receives research funding from the National Health and Medical Research Council of Australia and the Australian Research Council.
This article was originally published on The Conversation. Read the original article.