There was a "small possibility" a seven-year-old girl who died of sepsis after waiting almost two hours to be admitted to Perth Children's Hospital (PCH) might have lived if she had received care sooner, a coronial inquest has found.
The state's deputy coroner has handed down her long-awaited findings into the death of Aishwarya Aswath after her parents brought her into the hospital's emergency department (ED) one afternoon in April 2021.
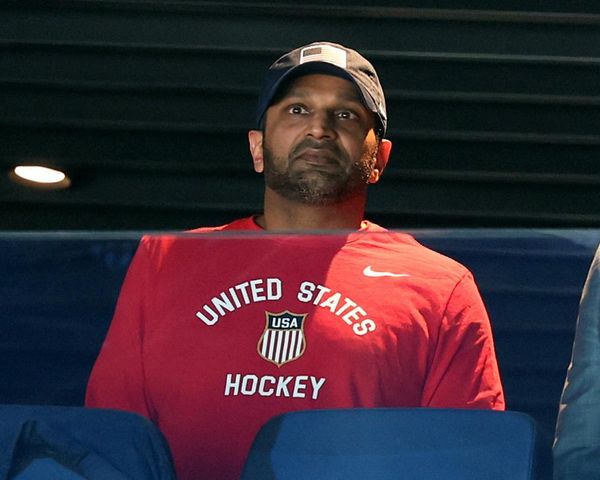
Aishwarya's parents Aswath Chavittupara and Prasitha Sasidharan, through their lawyers, said the findings had produced "mixed emotions".
"It has been incredibly upsetting for them to read what they have always known, that Aishwarya was deprived of the chance of survival by a series of missed opportunities as a result of systemic problems at Perth Children’s Hospital," the statement said.
"However, Aswath and Prasitha are also grateful that the Deputy State Coroner has taken the time to consider all of the evidence presented to the court, and arrive at the conclusion that the health system tragically failed Aishwarya and her family on that fateful day.
"Their mission has always been to ensure that Aishwarya’s death was not in vain and that improvements are made so that no other family has to endure what they have.
"We would urge the government to make sure that the Deputy State Coroner’s five recommendations are implemented as soon as possible."
Coroner Sarah Linton's recommendations included mandated patient-to-staff ratios in all public hospitals and a dedicated resuscitation team to be stationed at PCH emergency.
Other measures included changes to the records keeping system in state hospitals and new triage policies.
Aishwarya's parents have previously said they would "never forgive" the WA Health system but stressed they wanted the focus put on that system rather than individuals working within it.
Ms Linton commended their bravery and unwavering commitment in seeing the process through.
She also recognised many of the staff who gave evidence at the inquest were "deeply affected" by Aishwarya's death.
And while she noted many changes had been implemented in the wake of Aishwarya's death, she said it should not have come at such a cost.
"It shouldn't take the death of a beloved little girl for the Department of Health, and the government, to stop and consider what more it can do, and how much more money it should spend, to keep children safe when they visit our specialist children’s hospital."
WA Health Minister Amber-Jade Sanderson said the government had already started implementing most of the coroner's recommendations after Aishwarya's death.
Tragic missed opportunities
On 3 April 2021, the family had become worried by Aishwarya's listlessness, fever and very cold hands.
Nonetheless she was triaged at a relatively low priority and asked to go to the ED waiting room before she could be seen by a doctor.
What happened next has been described as a "cascade of missed opportunities" as staff failed to notice her quietly deteriorating despite her parents' best efforts to raise the alarm.
On Friday Ms Linton said the tragedy could have been prevented "if she had been given urgent medical treatment shortly after she first arrived at PCH".
Urgent healthcare reform recommended
Ms Linton recommended all public hospitals implement a 1 to 4 nursing staff-to-patient ratio advocated by Australian Nursing Federation (ANF), with particular priority given to EDs.
The coronial inquest last year heard from frontline staff, including the nursing shift coordinator, that the nurse to patient ratio in the ED was "insane".
Since Aishwarya's death the WA government has spent $20.5 million on the ED to hire another 46 nurses, doubling the existing team.
The nurses union made patient-to-staffing ratios part of their recent contract negotiations.
The WA Government last year committed to phasing in the ratios over two years, down from the three years initially put on the table.
Ms Linton said there was no reason the ratios could not be actioned earlier as "a matter of priority".
"Patient safety should not wait for the outcome of such [union and government] negotiations when the department of health's own independent inquiry supports such a change," the coroner said.
Ms Sanderson says four out of five of the recommendations are already being acted on, including boosting nurse-to-patient ratios before pay negotiations with nurses are concluded.
Dedicated resuscitation team needed
Ms Linton recommended the Child and Adolescent Health Service (CAHS), which is responsible for PCH, implement a dedicated resuscitation team.
The inquest last year heard from the nurse who assessed Aishwarya while she was in the waiting room was also filling an informal role as a "floater nurse" and her assessment was interrupted by other tasks.
She was required to attend an emergency resuscitation incident before completing her assessment which left Aishwarya unattended in the waiting room.
An independent review recommended a dedicated resuscitation team be put in place, however a hospital executive told the inquiry the positions were funded but had not been filled amid a difficult recruiting environment.
The health minister said a team was now in place and fully staffed.
Government not doing enough: union
Australian Nursing Federation WA secretary Janet Reah said the coroner's report backed up concerns the union had raised about ratios, but the government was not doing enough to fill empty positions.
"The thing that disgusts me the most isn't the fact that it took this death to put a light on the conditions ... what's really getting me is that nothing has changed in the two years since Aishwarya passed away," Ms Reah said.
She said the government had not yet delivered a "dedicated and supernumerary" team, which would include excess numbers of nurses standing by in the resuscitation bay.
"And they keep putting their hands up, saying 'we can't recruit'. It's not good enough. You've had two years to find nurses for those roles."
Death has led to 'significant changes'
The coroner's findings and recommendations have been accepted by the Child and Adolescent Health Service (CAHS), which runs PCH.
CAHS board chair Rosanna Capolingua said Aishwarya's death had led to significant changes within the health system, but conceded recruitment of new staff remained an issue.
She said there was a supernumerary resuscitation team at PCH's emergency department, but that team ended up plugging holes in the ED roster when not busy.
"The resuscitation team is a designated group of four nurses and their primary job is resuscitation," Dr Capolingua said.
"However, when there is no resuscitation, they can fall back and work in the ED to support the rest of the nursing team."
This meant there was no overall reduction in nursing staff on the floor when a resuscitation was needed, she said.
"We need to be recruiting more nurses, there is no doubt about that. That work of recruitment is absolutely continuous."
She was supportive of measures to support staff at PCH and improve patient outcomes.
"We remain steadfast in our commitment to continuous improvement in health care, and in supporting our staff to provide high quality safe care," she said.
'Safe harbour' for nurses who blow whistle on employers
In the wake of Aishwarya's death, hospital management reported three nurses and a doctor to the national medical worker watchdog, the Australian Health Practitioner Regulation Agency (APHRA).
The agency investigated but did not make adverse findings.
The Australian Nurses Union retaliated by referring hospital executive members to the agency for investigation, for failing to heed staff warnings that dangerous levels of understaffing were impacting patient safety.
The ANF said they met with the hospital's executive team in December, three months prior to Aishwarya's death, to raise concerns.
The coroner recommended the WA Government introduce "safe harbour" provisions to protect nurses from APHRA investigation and prosecution when an adverse event occurs where "known risks in the workplace have been identified and not rectified by the employer".
The inquest heard notes taken by nurses were in some cases not immediately transferred to digital systems, and there were multiple forms that needed to be filled out was said to add to the time, frustration and stress for nurses.
The health department said it was transitioning from paper to a state-wide electronic medical records system but coroner Sarah Linton said the government must prioritise funding these changes.
Changes to triage procedure
The triage nurse on duty the night Aishwarya arrived gave evidence she did not take observations such as heart rate or temperature.
At the time a large screen had been installed to reduce COVID transmission risk, and the intake desk put a distance between patients and the triage nurse.
Australasian College for Emergency Medicine guidelines do not require observations to be taken at triage, but the nurse said she had previously done so in other regional hospitals including Broome.
The hospital undertook a literature review following Aishwarya's death and determined there was no strong evidence that taking one or more vital signs at triage improved clinical outcomes.
However Ms Linton said it was her view that to prevent sepsis from being missed it was important to give priority to the first set of observations taken in children.
She recommended CAHS give consideration to implementing a new procedure for observations to be taken at triage or alternatively, within half an hour by the waiting room nurse, at PCH, when children present with gastrointestinal symptoms.
"This will ensure there is an early benchmark to measure the child’s progress and monitor for signs of sepsis," she wrote.
'Nurses and midwives are over-stretched'
The Australian Nurses Federation (WA) state secretary Janet Reah said in a statement she was pleased the coroner had adopted three recommendations from the ANF.
"It couldn't be clearer. Nurses and midwives are over-stretched and hospitals are drastically understaffed in both the public and private sectors," Ms Reah said.
"The community has had their faith severely shaken in the health system and this is reflected in the final statement by the coroner."
"There is no point in having a state-of the-art facility, if the staff working within it are stretched beyond capacity and parents lose their trust and faith in them."
Curtin University nursing professor Phillip Della said the recommendations were "solid and robust" and needed to improve the working lives of nurses and other health professionals.
"The recommendations are based on years of evidence that show that where we have safe staffing levels, patient care improves and the retention of our staff improves," Professor Della said.
Australian Medical Association WA president Mark Duncan-Smith says the WA government should extend the "safe harbour" provisions to doctors as well as increasing the operational budget of WA Health.
Premier not briefed on report
The WA Premier, Mark McGowan, spoke to ABC Radio Kimberley from Derby where he had been inspecting flood damage, and said he had not had a chance to read the coroner's report.
"I'll tell you everything I know, which is the health minister is commenting today on the report, she's had the opportunity to see it," he said.
"This trip has been booked for a while and I didn't know the report was coming down today, we only learnt about that late yesterday."
In a statement, Mr McGowan extended his "deepest sympathies" to Aishwarya's parents.
"What Aswath and Prasitha are going through must be unimaginable. It is something that no parent should have to go through," Mr McGowan said.
"Aishwarya will continue to leave a legacy – a lasting legacy – on our health system, on our hard-working staff who contribute to it each and every day and on the families who rely on it.
"The WA government takes this report very seriously, four of the five recommendations are underway and improvements continue to be implemented.
"The state government will continue to invest in our hospital system and do everything possible to ensure a tragedy like this is prevented from happening again."