Women health workers lost ground on equality during the pandemic, according to a new report from Women in Global Health.
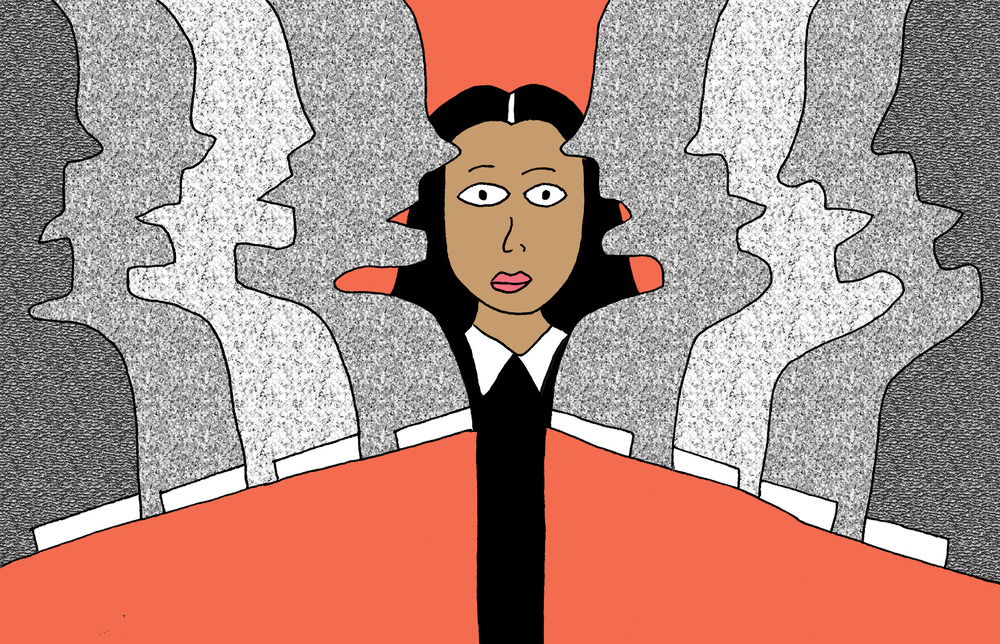
While 70% of the health care workforce around the world is made up of women, they hold only 25% of senior leadership roles, the report found – a phenomenon dubbed the "XX Factor."
Women had made some progress in closing the gender gap in leadership — until the pandemic. In 2020, for instance, the executive board of the World Health Organization reached a record 32% women, but then it fell to 6% in 2022.
"Wherever there is a high-profile emergency, these gendered stereotypes of leadership kick in even more than they do in normal situations," said Ann Keeling, senior fellow at Women in Global Health and lead author of the report.
Health workers were applauded as heroes, but during the pandemic, they faced longer hours, greater risks and more challenging work than ever, according to the report — as well as facing the pandemic-related challenges for women around the world, with massive additional burdens in childcare, education and elder or family care.
"COVID impacted women more than men in any sector, but particularly in the health and care sector," said Rosalia Vazquez-Alvarez, one of the authors of a 2022 report with the International Labor Organization on women in the health and care industries.
And, the new report found, women already marginalized because of their gender often faced even further discrimination based on age, race, religion, sexual orientation and other factors – being more frequently relegated to the lowest-paying and riskiest jobs. And this, says the report, is a crisis because inequality in health care will only make global health worker shortages worse – especially in less well-off countries.
While countries vowed in 2019 to close gender gaps like these, some countries may take more than 100 years to reach their goals if they don't change their approach, the report said.
The pandemic needs to be a "break in history" that makes us reevaluate what's important to us, Keeling said. "We don't have to keep relearning the same lessons."
Here are five obstacles the experts say stand in the way of gender equality in health care.
1. Men are still leaders in an industry dominated by women — and the pandemic made it worse.
Men headed up 85% of COVID task forces in 115 countries, according to the report.
"There was a very worrying dip in women's leadership during the pandemic," Keeling said. "The idea is 'there's an emergency, therefore men are better able to deal with this.' "
Women are often leading the charge to fight against viruses like COVID-19 in health care settings, but they are not afforded the respect, pay and safety of an official title, Keeling said.
That meant women were more likely to be excluded from making decisions based on their experience that would make patients' and providers' lives better, the report found.
For example, in some countries, safe maternity services were considered optional, not essential services in the pandemic. If there were midwives leading the response, they would undoubtedly have lobbied to keep these service going, as pregnancy and childbirth don't stop for a pandemic or any other emergency, Keeling explained. "We'd already learned that lesson in the Ebola pandemic."
Furthermore, there's a "broken pipeline" of health workers into leadership positions, where women are not seen within and outside of global health as political leaders and so they are not promoted nearly as often, the report said – making it more difficult to cultivate future generations of women in public health leadership.
Creating – and meeting – quotas for a certain number of women to fill leadership positions would help, the report said. Spain recently announced that large companies in several industries must have women represented in at least 40% of its top executives and management.
"If you have women at the very top, it may actually spill down" to other rungs of the industry, said Vazquez-Alvarez.
It's also crucial to value the work of women at every stage, she explains, "the people who are really taking care of the patients — the medical doctors, the surgeons, the nurses, the cleaners, et cetera."
2. The pandemic added to women's workloads.
"Women health workers suddenly found themselves with this huge spike in really sick patients," Keeling said, "working very, very long shifts, yet without access to their normal daycare for their kids."
Even as their workloads ballooned, their pay often did not – and their work at home, with virtual school and the care of young and elderly family members, increased. Women were expected to prop up the health care system while also holding down the home front, said Keeling – causing "a massive increase in stress."
Yet women receive little support for all of this extra work, the report finds. More family leave – sick leave, maternity leave, paternity leave, elder care leave — is necessary to close gender gaps, the researchers said. Some 72 countries, including the U.S., do not mandate at least 14 weeks of paid leave, putting childbearing women at a professional disadvantage.
And even at times when the flood of COVID patients subsides, health workers continue having huge workloads. People with other ailments may have deferred care during the past three years and now need to be seen. And broader initiatives like stalled vaccination campaigns needed to be restarted.
3. Women were more likely to be burnt out by the pandemic.
"It's not surprising now that what we see is massive exhaustion amongst the women who've been on the frontline for three years," said Keeling. "They're burnt out. But it's also to do with this concept of moral injury."
"Moral injury" in health care happens when health workers can't treat patients in a way that aligns with their values or professional training because the situation doesn't allow it – for instance, when patients die because hospitals run out of supplies, equipment, or life-saving treatments like oxygen. That can be devastating to watch or be a part of.
"The majority in patient-facing roles were really nurses, midwives, community health workers — so women suffered that highly traumatic moral injury," Keeling said.
Because there were more women on the front lines, they were more exposed to the virus and more likely to get sick, leading to death or disability from long COVID – a condition that early research shows tends to affect women more than men.
All of this means health care is now seeing a "great resignation" from women across the field. And women may begin looking for better-paying jobs in other countries, creating staff shortages in the places they're leaving, Keeling said.
There was already a shortage of 10 million health workers before the pandemic, according to the report. "We should be doing everything that we can to keep every trained woman in the health workforce," Keeling said.
4. Much of the caretaking work done by women in health care is informal and poorly paid.
An estimated 6 million women in the health workforce are not paid at all or "grossly underpaid," the report said. Community health workers might receive a cell phone or a bicycle instead of money for their work – and these workers tend to be women.
The gender pay gap is higher in health care than in any other economic sector in the economy – around 25%, Vazquez-Alvarez said. "For each dollar a man makes, a woman makes 75 cents." And most of this gap can't be explained away by age, education, or experience, she said.
COVID hasn't made this any better. "If anything, the gender pay gap in the health sector is likely to have increased," said Vazquez-Alvarez, who is working to quantify such gaps now.
But the problems around informal work go beyond money.
Informal workers don't have access to social safety nets, like unemployment and other benefits, and it can be harder for them to advance within health care. For example, says the report, in India, the community health workers known as ASHAs (Accredited Social Health Activists) can't take family leave or report sexual harassment complaints.
"We have millions of women working in health who are not part of the formal health system, and that means they can never progress from where they are," Keeling said. "They're community health workers, but they have no opportunity to progress to become nurses or to become anything else in the hierarchy — but they're leaders in their own right."
5. The workplace in health care is geared toward men.
The gender divide can affect everything from advancement opportunities to daily work.
Personal protective gear, or PPE, for example, was designed for male bodies – which means they can fit women poorly, increasing the risk of infection.
In the pandemic, workers often had to wear full-body PPE all day, which meant they couldn't use the bathroom for entire 12-plus-hour shifts. For menstruating, breastfeeding, and pregnant workers, poorly designed PPE was a major challenge. It meant they couldn't change sanitary pads, pump breast milk, or urinate regularly – which can lead to health issues.
"We've been working since with the manufacturing standards bodies for medical PPE to make sure that this is taken seriously and that they get this right the next time," Keeling said.
The struggle to even get PPE revealed deep gender inequality. Women were often "the lowest in the hierarchy and they were the last to get PPE," Keeling said. ASHAs in India went on strike in 2021 to demand better conditions, including access to PPE – but their calls basically went unheeded and they returned to work.
Policies on sexual abuse and exploitation of women in health care also don't go far enough, researchers say, and 41 countries don't have bans on firing women just for being pregnant.
These examples show how widespread inequality is, and how collective action could help keep women safe and able to keep working, Keeling said.
"Try to understand, when nurses go out in the streets and try to fight for better earnings, it's social justice, [and] it's a way to also compensate these people — our lives are in their hands," Vazquez-Alvarez said.
What is the path forward?
Gender inequality is a longstanding issue, and so many of the solutions are familiar – they just need to be implemented.
Collective action and organizing for better conditions are an important step to begin changing the system, Keeling said, and so is adding quotas to make sure women are well-represented among health leaders. Guaranteeing parental and family leave to all workers is also key, as well as paying all workers fairly, she said.
All genders need better education about gender and health care, Vazquez-Alvarez said – for instance, more encouragement for men to pursue nursing and for women to become doctors.
"It's not about fixing women to fit into systems that discriminate against them, it's really about fixing the systemic bias that doesn't really see women as leaders," Keeling said.
Melody Schreiber (@m_scribe) is a journalist and the editor of What We Didn't Expect: Personal Stories About Premature Birth.







