A woman who has undergone a pioneering gene-editing treatment on the NHS is optimistic that 2026 will mark the year she is cured of a severe blood disorder.
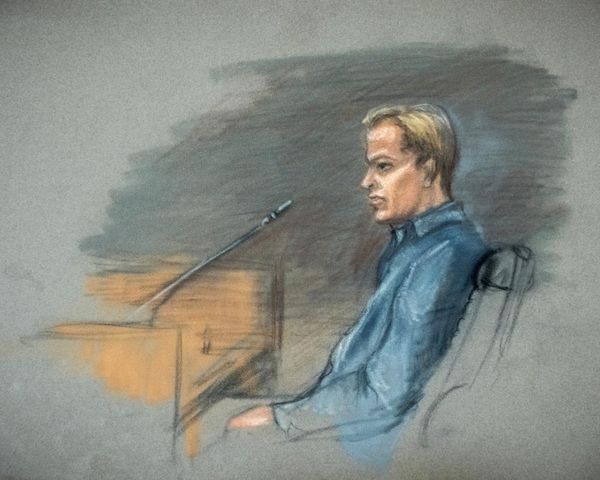
Kavita Mehta, 36, from London, suffers from beta thalassaemia, a genetic condition preventing her body from producing sufficient haemoglobin – the vital protein in red blood cells responsible for oxygen transport.
This inherited disease necessitates blood transfusions every three to five weeks for patients, significantly shortening their life expectancy.
Ms Mehta has relied on transfusions and medication throughout her life to survive.
But now she has become one of the first patients in the south of England to receive the gene-editing treatment Casgevy on the NHS.
She underwent her treatment in November and is now at home recovering – with all the signs pointing to the fact she may be experiencing a cure.
Ms Mehta, who works as a director of rooms in the hospitality industry, was diagnosed with beta thalassaemia when she was one month old.
“We were living in Kenya at the time,” she explained. “My grandmother noticed I looked unusually pale, my mum took me to hospital, and that’s when they found out.
“My parents are both carriers and so is my brother. I started transfusions straight away. I can’t remember how many bags I needed, but from the beginning it was every six weeks without fail. That carried on for years.
“When I was five, I began iron chelation (a treatment to remove extra iron from the blood caused by blood transfusions). That was the hard part.
“The needles back then were awful – huge butterfly needles – and my poor mum had to give me the injections every night.
“Iron chelation used to be a slow 10-hour overnight infusion, five nights a week.
“It dictated everything – my weekends, school mornings, even nights out when I got older.”

Ms Mehta has also experienced a lifetime of tiredness and pain in the week leading up to her blood transfusions, which could now be a thing of the past thanks to Casgevy.
“As you get closer to needing a transfusion, you feel it,” she said.
“I get out of breath, my chest pounds, my head aches, and even my lower back hurts.
“It’s eased as I’ve got older, but as a child and in my 20s it used to hit me hard. I avoid the gym the week before a transfusion because I simply can’t cope. I slow down until I’m back in hospital topping up again.”
With Casgevy, blood stem cells are removed from the patient’s body and edited in the lab before being returned to the patient via an infusion.
The technique relies on a tool called Crispr, an award-winning method for targeting DNA and performing an edit.
Shortly after people are born, foetal haemoglobin starts to be replaced by adult haemoglobin.
But for people with beta thalassemia, their bodies are not able to make enough working adult haemoglobin.
Casgevy overcomes this by switching on foetal haemoglobin production, which enables the body to overcome beta thalassaemia and offers the chance of a cure.
Before undergoing treatment, patients are given an intensive course of chemotherapy.
They then need to stay in hospital for around six weeks to allow the genetically-edited stem cells to embed and flourish.
After receiving Casgevy in November at University College London Hospital (UCLH), Ms Mehta is now recovering at home.
“I feel fine now, I’m back to chores and I’m walking around,” she told the Press Association.
“It’s looking really good. Even when I was in the hospital, things were looking really good.
“My foetal haemoglobin is kind of holding steady and increasing – which obviously would never have happened before.
“So in the doctors’ eyes, it it is working. It’s incredible and it’s crazy.
“Honestly, I just keep thinking these scientists who discovered this whole procedure are just geniuses.
“To change a whole group of people’s lives is incredible.
“I’m under the NHS, and I was one of the first people in the South so I know that I’m very lucky, but I hope more people will have access to Casgevy.”

Ms Mehta said she is looking forward to being able to travel more and live a normal life.
“I’d love to travel for longer than four weeks, that would be amazing,” she said.
“I’ve heard some people say that your energy levels just increase tenfold, and you never feel that kind of slump after three two to three weeks (like before), which is very exciting for me.
“You have to be transfusion independent for one year to be cured, but that is my hope.”
Ms Mehta and her husband, who does not wish to be named, have also undergone fertility treatment to freeze embryos in the hope of starting a family in the future. The chemotherapy treatment she needed before Casgevy affects fertility.
The couple have been told to wait two years before conceiving, but Ms Mehta said: “With my bloods being so good, they’re saying in a year, if my bloods are still the same, that they see no reason not to start. So that’s quite exciting.”
She added: “A life of regular blood transfusions is all I know.
“I cannot believe that doctors have already seen signs that I am now able to produce my own red blood cells.
“I can’t tell you what this means to me, and to my family who have had to watch me go through this and care for me.
“And more than anything, I am thrilled that this drug is available on the NHS and may help patients who are much younger than me live a life independent of transfusions.”
In international clinical trials, Casgevy has shown impressive results, removing the need for blood transfusions for at least a year in 93 per cent of patients.
UCLH haematology consultant Dr Ben Carpenter, who has been treating Ms Mehta, told PA: “We are pleased with the way things are going.
“It has been more than two weeks since Kavita’s last red cell transfusion, and her levels are continuing to rise independently.
“We are now seeing normal red blood cells being produced by her own bone marrow for the first time since she was born.”
He described the success rate for Casgevy as “fantastic”, adding: “It really is a game-changer for the transfusion dependent thalassemia community.”
He said the therapy is a “a beautiful solution for these conditions”, adding: “It does look like it is a curative treatment”.
Woman with blood disorder hopes for cure thanks to NHS gene-editing therapy
We’re making headway on reducing NHS waiting times, says Swinney
How millions of people go to A&E for minor problems like a headache or blocked nose
NI health service problems would become more acute, official warned in 2005
The ‘transformative role’ pharmacies could have in HIV prevention