Support truly
independent journalism
Our mission is to deliver unbiased, fact-based reporting that holds power to account and exposes the truth.
Whether $5 or $50, every contribution counts.
Support us to deliver journalism without an agenda.

Louise Thomas
Editor
Cervical cancer screening tests could soon be done at home – in a move experts say would be game changing.
NHS leaders are looking at making quick and easy-to-use self-testing kits available in England, leading to around 400,000 more people being tested every year.
The test detects human papillomavirus (HPV), a group of viruses which cause no symptoms but which can lead to cervical cancer. About 13 high-risk types of HPV are known to cause 99.7% of all cervical cancers.
Figures show cervical screening uptake is declining, particularly among younger women. Testing may be missed due to a lack of convenient appointments, embarrassment and worries about the test causing pain.
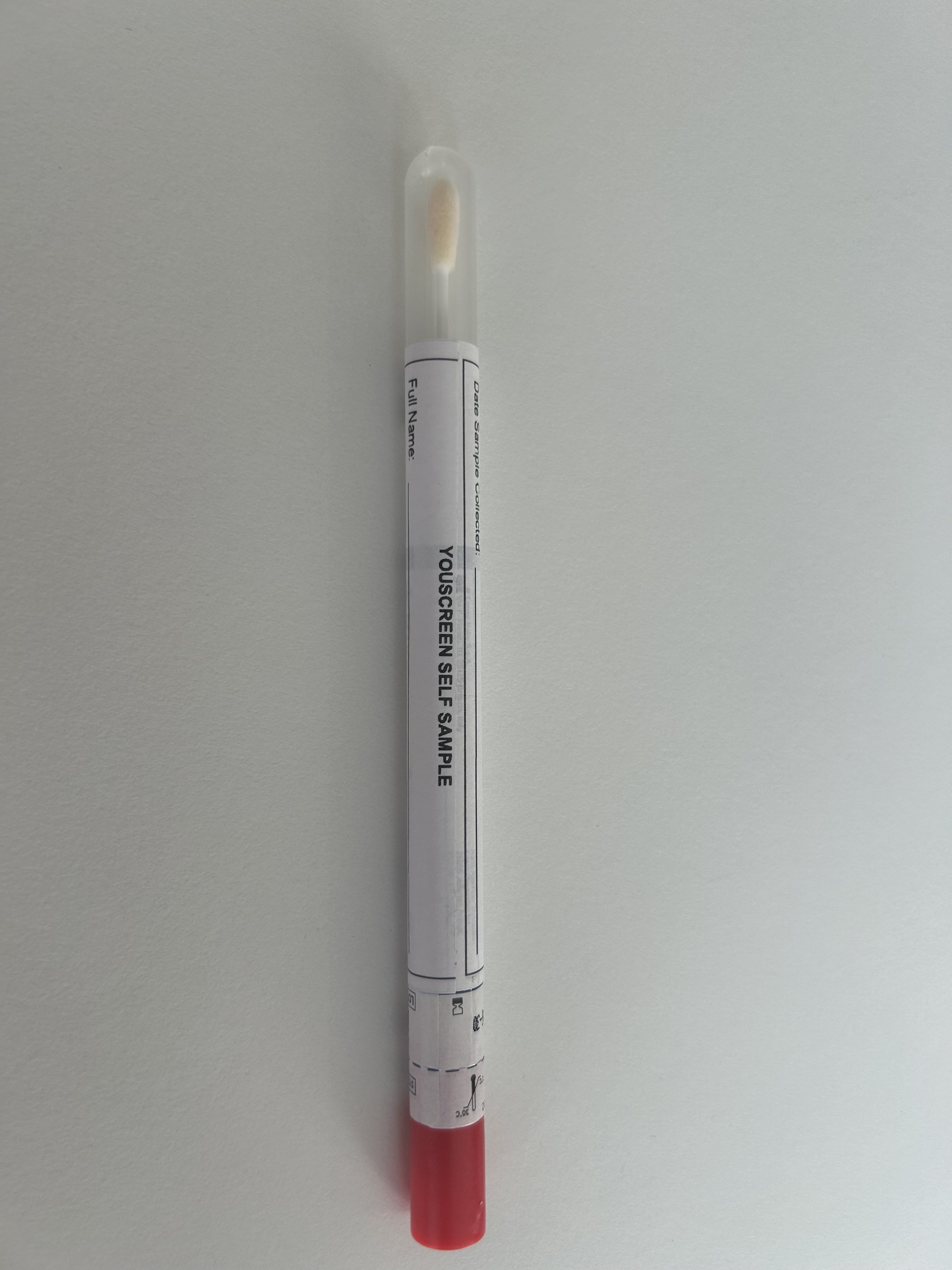
In the King’s College London YouScreen trial, the biggest to date, women used a vaginal swab – like a long cotton bud – to take a sample themselves, either at home or in their GP practice, before posting their kit off for free to a laboratory.
Other countries such as the Netherlands, Australia, Denmark and Sweden have already introduced the self-testing kits.
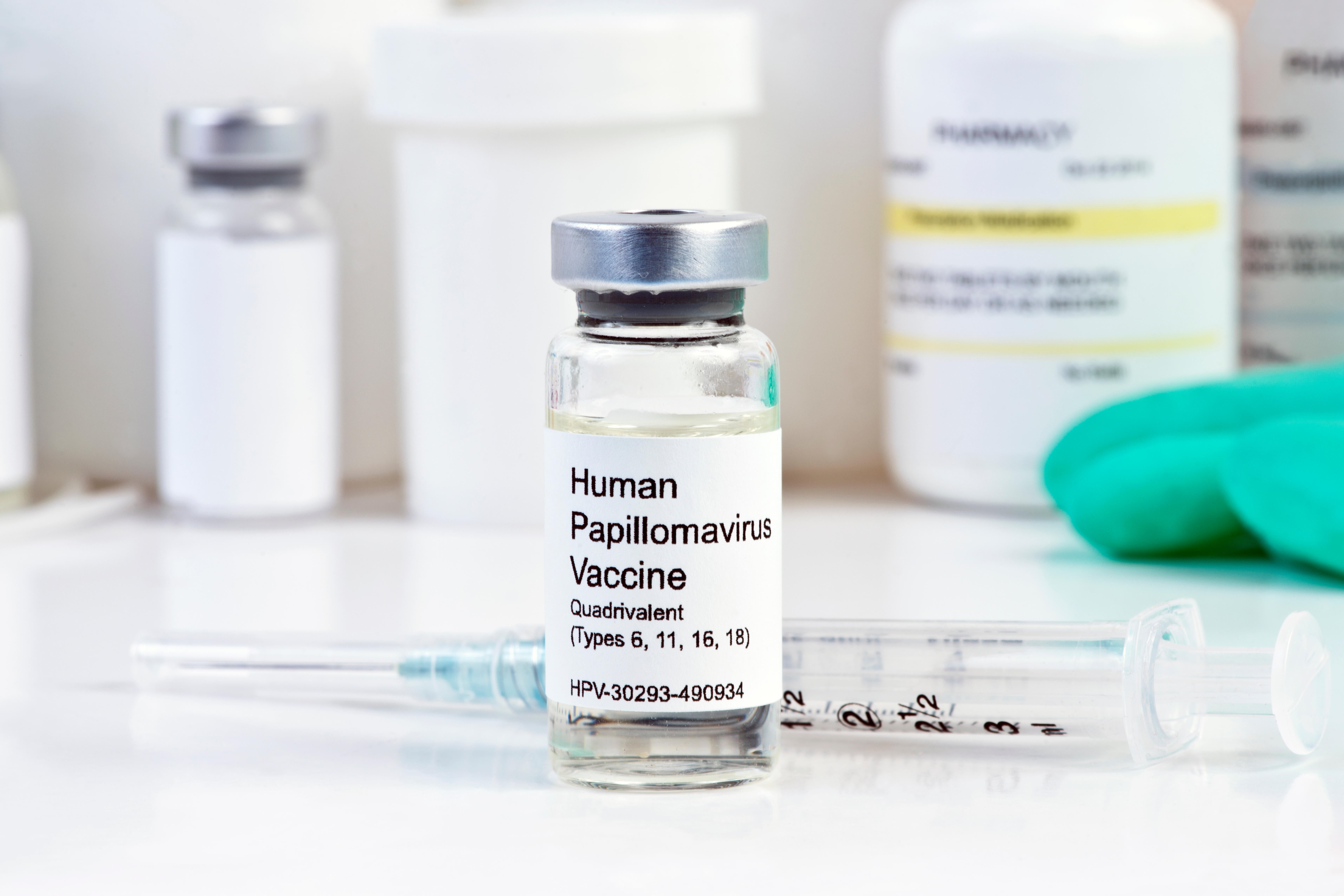
The introduction of an HPV jab is helping to prevent cervical cancer but women who haven’t been vaccinated still need to attend screening every three to five years depending on their age.
What is cervical cancer?
Cervical cancer is a cancer found anywhere in the cervix – the opening between the vagina and the womb – and is usually caused by an infection from certain types of human papillomavirus (HPV), according to the NHS.
Most people will get HPV at some point in their lives and it usually goes away without causing any problems, but high-risk HPV sometimes causes changes in the cells of the cervix, which can slowly develop into cervical cancer.
What are the symptoms?
According to the NHS, the most common symptoms can include vaginal bleeding that is unusual for you, including after the menopause, after sex, or between regular periods; changes to vaginal discharge; pain or discomfort during sex; and unexplained pain in your lower back or between your hip bones.
But cervical cancer may not cause any symptoms or the symptoms may not be obvious, says The Eve Appeal.

Who is most at risk?
Anyone with a cervix can get cervical cancer, but it mainly affects women under the age of 45, according to the NHS.
Some factors might make you more likely to get cervical cancer. These include a weakened immune system, giving birth to multiple children or having children when you were under 17, having a vaginal, vulval, kidney or bladder cancer in the past, or your mother took the hormonal medicine diethylstilbestrol while pregnant with you.
Can you do anything to minimise your risk?
Attending cervical screenings and getting the HPV vaccination, available from the age of 12 or 13 up to 25, are the best ways to protect yourself from cervical cancer. It’s best to have the vaccine before having sex for the first time.
You can also lower your chance of getting cervical cancer by using condoms, quitting smoking – as smoking can weaken your immune system and the chemicals in cigarettes can also cause cervical cancer – and eating a balanced diet, which helps support your immune system.
How it it currently diagnosed?
If you have symptoms, you should be offered a pelvic examination, which often involves a GP pressing your stomach to feel for anything unusual, and looking inside and outside of your vagina.
If a screening shows you have abnormal cells in your cervix, you’ll usually be referred for a colposcopy to have a closer look at your cervix.
Then, you will usually be invited to the hospital for an appointment with a consultant oncologist to explain the test results and next steps, as well as answer any questions you might have.
Macmillan Cancer Support also notes that cervical cancer may also be diagnosed during cervical screening or after an abnormal smear test – while this isn’t common, it sometimes happens.
How is it treated?
Treatment can include chemotherapy or radiotherapy, but surgery is often the main treatment for cervical cancer, especially if the cancer is found early.
Different surgeries include removing part of the cervix, or a hysterectomy – removing the cervix and the womb.