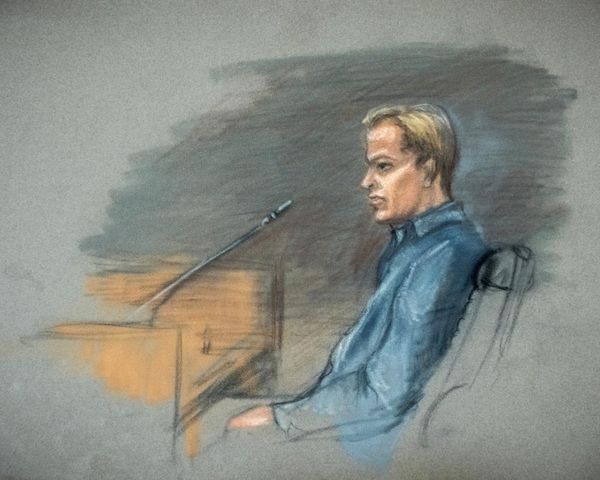
Penny Rowden was among the first Australians to catch COVID-19 back in early 2020, but she still has not fully recovered.
"When you're a healthy person, as you age, you expect to get less healthy, but when you're hit by something like this and you feel so terrible, you just feel as though that's the end really," Ms Rowden said.
The 74-year-old contracted the virus while on a bus full of tourists at Rottnest Island off Perth's coast.
A few days later, she began feeling sick, showing symptoms of severe fatigue and weakness, high temperature, shakiness, brain fog, loss of taste and smell and a heavy cough.
Those symptoms persisted for more than a year.
"I went back to my doctor every couple of weeks for six months and was given a total of nine courses of antibiotics," she said.
"I couldn't go out of the house because I was coughing all the time, so I had no social life.
"I lost about 15 kilograms and ended the year on anti-depressants … I was living a semi life."
Long COVID still misunderstood
Ms Rowden is one of many long COVID sufferers advocating for more attention to the condition and for easier community access to health professionals.
Long COVID clinics have been set up in major hospitals in most states and territories, offering services such as rehabilitation, physiotherapy and psychological support.
However, Western Australia continues to remain without one.
Now a group of medical professionals in Perth is hoping to change that.
Physiotherapist Jo Milios decided to take matters into her own hands after noticing an increase of old patients returning with random symptoms after their COIVD-19 infection.
"Normally what happens is, once they're fixed and cured, you don't see them again," Dr Milios said.
"I wanted to see whether or not this was a problem, so I started screening my patients, asking them if they'd had COVID, if they'd had the vaccines, and whether or not they had any side effects … and it came to be about one-in-three people were still demonstrating problems.
"Various people were getting tachycardia, the fitter they were, the quicker they seemed to crash and the longer they seemed to be burdened by symptoms."
Dr Milios contacted her colleagues and found that they were also noticing similar patterns.
"I started gathering a list of what I call 'COVID-compassionate' health professionals, and that can be anything from cardiologists to respiratory physicians to endocrinologists to urologists … there's [more than] 200 potential symptoms that we need to address," she said.
"They were all keen to assist by making sure we triage people appropriately to the right destination person."
Kicking long COVID together
The group has begun community workshops as part of their rehabilitation program called "Kick! Long COVID".
In partnership with Emerge Australia, the program is aimed at helping to educate the public and other health professionals about the condition.
Dr Milios says it can be a blueprint model for the rest of the country to fill the gaps in understanding long COVID and how it can be prevented.
"I'm hoping that, through this little bit of discussion and conversation, we get to be the best place in the world to respond to this, because we've got the resources [and] we've got a great community," she explains.
"We also have a $6 billion profit margin once again here in Western Australia and it would be good if some of that could be allocated to [this]."
Education about long COVID prevention
While there's no specific clinic yet, Dr Milios and her colleagues have already begun treating patients with long COVID symptoms and teaching others about how to prevent it.
"We don't really know what we're doing, because it's all new," she said.
"But what I think that we failed to do in the medical system was [to] recognise that you actually need to do what the World Health Organization recommended, and that is to stop, rest and pace your recovery."
That advice was the saving grace for Tony Jones, one of Dr Milios's patients and the captain of Hockey Australia Masters Men's 60s World Cup Team.
Mr Jones struggled with debilitating symptoms after his COVID-19 infection earlier this year, putting his sports career at risk.
"I developed a really heavy chest and cough, and it's taken a long time, a lot of antibiotics, lots of doctor's visits and seeing specialists and other people just to try [to] work out why this keeps happening and why I'm not recovering," he said.
While he was initially reluctant to put his fitness on hold, a couple months of rest was the key to helping Mr Jones get back on his feet and recover enough to play in the Tokyo World Cup.
"The experience I suppose helps you learn about your own body and how it works," he said.
"Sometimes, we do need to stop, take a step back and just go, 'Am I really feeling okay?'"
Call for more research on condition
With thousands of people expected to develop long COVID in Australia, GPs say more data is needed.
The West Australian chair of the Royal Australian College of General Practitioners, Ramya Raman, said it was challenging for doctors to diagnose the condition without a complete understanding of it.
"It's very important, because we are seeing it in the community," she said.
"The more we know about it, the better we can actually manage the condition and [be] better informed."
A parliamentary inquiry into long COVID is currently underway to investigate the economic, social, educational and health impacts the condition and repeat infections.
In Western Australia, the Department of Health intends to survey people who have been diagnosed with the virus to help shape what resources and future health care needs the state would require for long COVID.
Dr Raman said that, as the numbers continued to rise, a long COVID clinic should be considered to help patients access health professionals under one roof.
"The dedicated clinics have been helpful for a lot of my eastern state colleagues, and I think it would be helpful here in Western Australia as well … having the initial screening and the testing being done to actually analyse and review this," she said.
Penny Rowden says a clinic in Perth would have helped her get answers sooner.
"You feel so much on your own. You feel as though nobody else knows what you're going through," she said.
Ms Rowden still has some ongoing symptoms and was diagnosed with bronchiectasis last year.
She hopes to see educational programs such as Jo Milios's implemented across the country to support those who have the condition.
"I just want to get the message across to people that there is such a thing as long COVID and there is help available," she said.