
Around 15% of the world’s population suffers from tinnitus, a condition which causes someone to hear a sound (such as ringing or buzzing) without any external source. It’s often associated with hearing loss.
Not only can the condition be annoying for sufferers, it can also have a serious effect on mental health, often causing stress or depression. This is especially the case for patients suffering from tinnitus over months or years.
There’s currently no cure for tinnitus. So finding a way to better manage or treat it could help many millions of people worldwide.
And one area of research that may help us better understand tinnitus is sleep. There are many reasons for this. First, tinnitus is a phantom percept. This is when our brain activity makes us see, hear or smell things that aren’t there. Most people only experience phantom perceptions when they’re asleep. But for people with tinnitus, they hear phantom sounds while they’re awake.
The second reason is because tinnitus alters brain activity, with certain areas of the brain (such as those involved in hearing) potentially being more active than they should be. This may also explain how phantom percepts happen. When we sleep, activity in these same brain areas also changes.
Our recent research review has identified a couple of brain mechanisms that underlie both tinnitus and sleep. Better understanding these mechanisms – and the way the two are connected – could one day help us find ways of managing and treating tinnitus.
Sleep and tinnitus
When we fall asleep, our body experiences multiple stages of sleep. One of the most important stages of sleep is slow-wave sleep (also known as deep sleep), which is thought to be the most restful stage of sleep.
During slow-wave sleep, brain activity moves in distinctive “waves” through the different areas of the brain, activating large areas together (such as those involved with memory and processing sounds) before moving on to others. It’s thought that slow-wave sleep allows the brain’s neurons (specialised brain cells which send and receive information) to recover from daily wear and tear, while also helping sleep make us feel rested. It’s also thought to be important for our memory.
Not every area of the brain experiences the same amount of slow-wave activity. It’s most pronounced in areas we use most while awake, such as those important for motor function and sight.
But sometimes, certain brain areas can be overactive during slow-wave sleep. This is what happens in sleep disorders such as sleep walking.
A similar thing may happen in people with tinnitus. We think that hyperactive brain regions might stay awake in the otherwise sleeping brain. This would explain why many people with tinnitus experience disturbed sleep and night terrors more often than people who don’t have tinnitus.
Tinnitus patients also spend more time in light sleep. Simply put, we believe that tinnitus keeps the brain from producing the slow-wave activity needed to have a deep sleep, resulting in light and interrupted sleep.
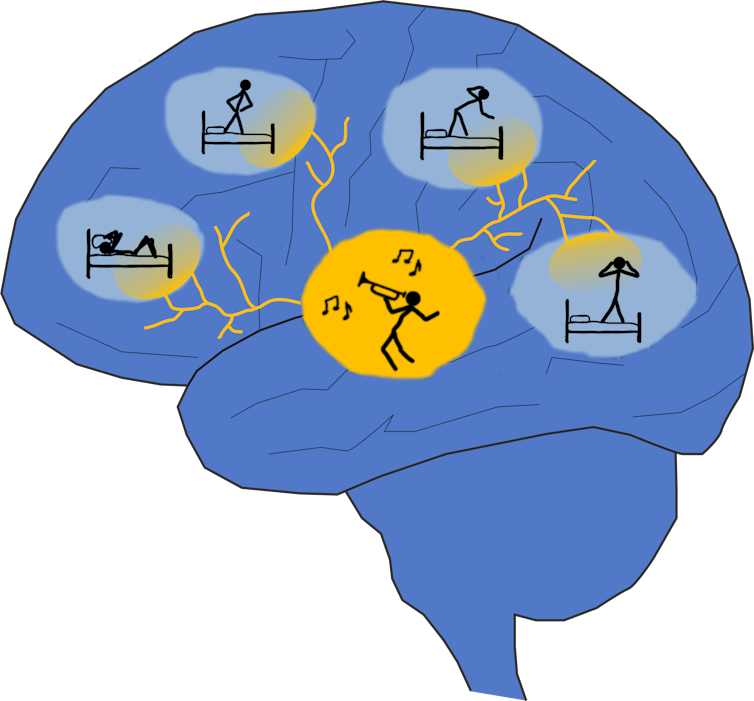
But even though tinnitus patients have less deep sleep on average than people without tinnitus, the research we looked at in our review suggests that some deep sleep is hardly affected by tinnitus. This may be because the brain activity that happens during the deepest sleep actually suppresses tinnitus.
There are a couple of ways the brain may be able to suppress tinnitus during deep sleep. The first has to do with the brain’s neurons. After a long period of wakefulness neurons in the brain are thought to switch into slow-wave activity mode to recover. The more neurons in this mode together, the stronger the drive is for the rest of the brain to join.
We know that the drive for sleep can get strong enough that neurons in the brain will eventually go into slow-wave activity mode. And since this especially applies to brain regions overactive during wakefulness, we think that tinnitus might be suppressed as a result of that.
Slow-wave activity has also been shown to interfere with the communication between brain areas . During deepest sleep, when slow-wave activity is strongest, this may keep hyperactive regions from disturbing other brain areas and from interrupting sleep.
This would explain why people with tinnitus can still enter deep sleep, and why tinnitus may be suppressed during that time.
Sleep is also important for strengthening our memory, by helping to drive changes in connections between neurons in the brain. We believe that changes in brain connectivity during sleep are contributing to what makes tinnitus last for a long time after an initial trigger (such as hearing loss).
Treating tinnitus
We already know that intensity of tinnitus can change throughout a given day. Investigating how tinnitus changes during sleep could give us a direct handle on what the brain does to cause fluctuations in tinnitus intensity.
It also means that we may be able to manipulate sleep to improve the wellbeing of patients – and possibly develop new treatments for tinnitus. For example, sleep disruptions can be reduced and slow-wave activity can be boosted through sleep restriction paradigms, where patients are told to only go to bed when they’re actually tired. Boosting the intensity of sleep could help us better see the effect sleep has on tinnitus.
While we suspect that deep sleep is the most likely to affect tinnitus, there are many other stages of sleep that happen (such as rapid eye movement, or REM sleep) – each with unique patterns of brain activity. In future research, both the sleep stage and tinnitus activity in the brain could be tracked at the same time by recording brain activity. This may help to find out more about the link between tinnitus and sleep and understand how tinnitus may be alleviated by natural brain activity.
Linus Milinski received funding from the Royal National Institute for Deaf People (RNID).
Fernando Nodal's research is funded by the Wellcome Trust.
Victoria Bajo Lorenzana's research is funded by the Royal National Institute for Deaf People (RNID) and by the Wellcome Trust.
Vladyslav Vyazovskiy receives research funding from the Medical Research Council.
This article was originally published on The Conversation. Read the original article.







