In 1817, Jacob Parkinson, an English surgeon and polymath, published a brief, 66-page booklet on a condition that was little known to the medical community. In An Essay on the Shaking Palsy, Parkinson described, in excruciating detail, his observations of six individuals demonstrating varying degrees of the same symptoms: involuntary tremors, difficulty walking, muscle weakness, and slurred speech.
As you may have guessed, Parkinson was describing the disease now bearing his name, a neurodegenerative condition that affects nearly a million U.S. adults. Over the last two hundred years, we’ve since discovered the why behind the disease — destruction of neurons producing the neurotransmitter dopamine — and how to treat it through a variety of innovative means.
But doctors still struggle to diagnose Parkinson’s in the first place, particularly in its early stages. Scientists are aiming to change that with a new AI-powered device that can help diagnose Parkinson’s from breathing patterns, according to a paper published last month in the journal Nature Medicine.
Here’s the background — The Parkinson’s-detecting device relies on a technology called wireless sensor networks (WSNs), says Dina Katabi, a senior study author and professor in MIT’s Department of Electrical Engineering and Computer Science.
WSNs were first developed by the U.S. military in the 1950s to track Soviet submarines. Since then, we’ve used these networks of dedicated sensors to monitor a myriad of phenomena like air quality and natural disasters, or for military purposes such as gathering intelligence and pinpointing security threats.

Now, WSNs are increasingly making their way into health care. That’s because they’re far more convenient to collect health data compared to wearables that people keep on for extended periods to capture temperature, blood pressure, or other vital signs. On the other hand, WSNs deploy a group of sensors that can gather this information from a distance and relay it for processing.
For example, if you or a loved one lives in a care home, a smart environment of sensors may improve safety and quality of life. In emergency rooms, for example, WSNs could allow doctors to respond quickly the moment a patient’s condition deteriorates.
How they did it — Katabi and her team discovered that WSNs could analyze breath patterns during sleep to detect Parkinson’s disease.
“Our breathing during sleep changes and follows our sleep cycles,” explains Katabi. “When you’re in deep sleep, your breathing is different from when you’re in REM, for example.”
This decision is based on observations from James Parkinson himself back in 1817, along with data from recent studies. It turns out that Parkinson’s destroys neurons in the brainstem, where breathing is controlled.
Because nighttime breathing changes can manifest years before a person develops more obvious signs of Parkinson’s, they can reveal early brain changes or disturbances.
But how can a wall-mounted wireless sensor actually recognize changes that are imperceptible to the human eye? To do that, it had to get smart.
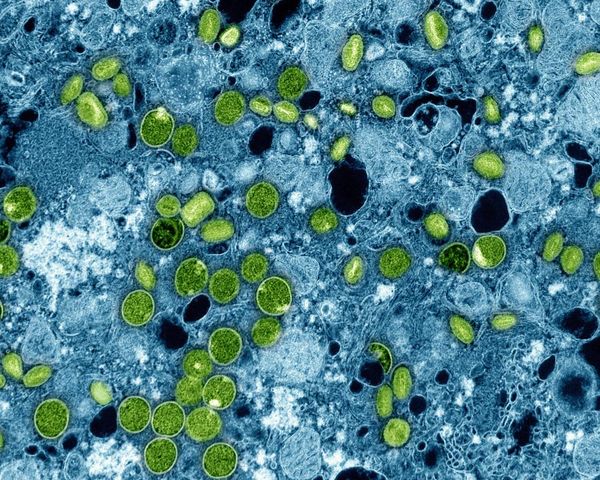
MIT graduate student Yuzhe Yang and postdoctoral fellow Yuan Yuan, both members of Katabi’s team, worked with a neural network that resembles a human brain via connected algorithms that reflect the behavior of actual neurons. They taught the network to recognize typical versus Parkinson’s disease-associated nocturnal breathing through 12,000 nights of sleep data from sleep labs across the U.S.
To pick up on breathing changes, the neural network — which is housed in a device that looks like your average WiFi router — uses echolocation, somewhat like how bats do it.
But instead of sound waves, the device sends out radio waves that bounce off the body, Katabi says. These altered radio waves return to the device and provide a picture of a sleeping person’s breathing patterns. The neural network then examines the “image” and offers its assessment.
What they found — Among the subjects with Parkinson’s, the AI focused on breath during sleep onset and awakening — this makes sense because people with Parkinson’s tend to have less deep sleep and more interruptions during their slumber. The device can also pick up on differences in a person’s breathing over time and indicate worsening cases. (This was tested on a large data set of 7,687 people, including 757 Parkinson’s patients.)
“The neural network not only is ... saying whether this person has Parkinson’s or not, [but] it’s also giving an estimate of the severity of the disease,” says Katabi. That’s important because the researchers want to track how quickly the disease is progressing in some people versus others, and why these differences exist.
Because other neurodegenerative diseases can bring overlapping symptoms, Katabi and her team wanted to make sure they were detecting Parkinson’s and not anything else. Based on data from people with Alzheimer’s disease, the AI showed a sensitivity of nearly 81 percent. In telling Parkinson’s disease apart from Alzheimer’s, it had a specificity of 78 percent.

Why it matters — Currently, we don’t have any non-invasive methods that can detect the early stages of Parkinson’s disease. And during clinical drug trials, researchers rely on imprecise questionnaires, or a combination of questionnaires and tasks, to judge how a participant’s doing or measure how their disease is progressing.
“[These means] are subjective or semi-subjective and also not sensitive,” says Katabi. “That lack of sensitivity, in the current methods, makes it difficult to have clinical trials for Parkinson’s disease that detects more changes in the disease,” and recruit people for such clinical trials.
There’s also the burden of Parkinson’s disease that’s driven by more of the population leading longer lives. From 1990 to 2015, the number of people with Parkinson’s doubled to over 6 million, a number expected to double again to over 12 million by 2040.
Rising rates of Parkinson’s come with a high price tag: The total economic burden of the disease is estimated at nearly $52 billion, according to one 2020 Nature study. While we don’t have a cure for Parkinson’s just yet, early detection could bring down health care costs.
What’s next — Since smart devices already run our households (and our lives), this Parkinson’s disease-detecting AI sounds like a highly practical gadget to add to the roster.
And Katabi envisions more diagnostic tools in the future. For instance, the AI could even recognize the smell of Parkinson’s disease and distinguish between specific types of the condition (right now it's more of a general sweep).
It could also be programmed to recognize Alzheimer’s disease, amyotrophic lateral sclerosis, and other neurodegenerative diseases that are hard to find in the nascent stages — offering hope for those with these elusive conditions.