
For years, scientists have wondered how migraines can trigger auras — short-lived neurological symptoms that arise before or during migraines. Now, a newly discovered way in which the brain talks to peripheral nerves may be the answer, a mouse study suggests.
More than 1 billion people each year will have a migraine, and about one-quarter of those migraines will be accompanied by an aura. These sensory symptoms can include seeing lights and hearing sounds that aren't there or feeling tingling or numbness.
Scientists have known that these auras are associated with "cortical spreading depression," waves of abnormal activity that wash over the brain and temporarily inactivate certain neurons. The waves are thought to somehow trip pain-detecting nerves outside the brain, in part by releasing chemicals into the cerebrospinal fluid (CSF), a substance that surrounds and cushions the organ.
Exactly how the chemicals reached the nerves was a mystery. Now, scientists have uncovered a route by which some molecules can escape the brain's protective barrier.
Related: Migraines and blood sugar issues share common genetic risk factors
In a study published Thursday (July 4) in the journal Science, researchers examined the route CSF takes to exit the brain by zooming in on a cluster of neurons called the trigeminal ganglion. This bundle of cells transmits signals from the nerves of the face and jaw to the brain, plugging in around the brainstem.
The scientists discovered that this nerve bundle also provides a route for CSF and the molecules within it to reach the world beyond the brain.
They learned this by using genetically engineered mice whose neurons make a protein that glows in the presence of calcium. Calcium is a key element that brain cells use to send electrical signals. While observing the trigeminal ganglion, the researchers would inject a tracer into the mouse's brain to track the flow of its CSF. They also introduced a substance that allows calcium to flow into neurons, activating them.
The experiment revealed that CSF appeared in the trigeminal ganglion about four minutes after injection, followed by a sharp increase in calcium-driven activity. This provided direct evidence that CSF can carry molecules outside the brain via this channel.
The fluid likely makes contact with the ganglion near the brainstem. There, the ganglion lacks the tightly fused outer barrier that can be seen elsewhere along its length, the team found.
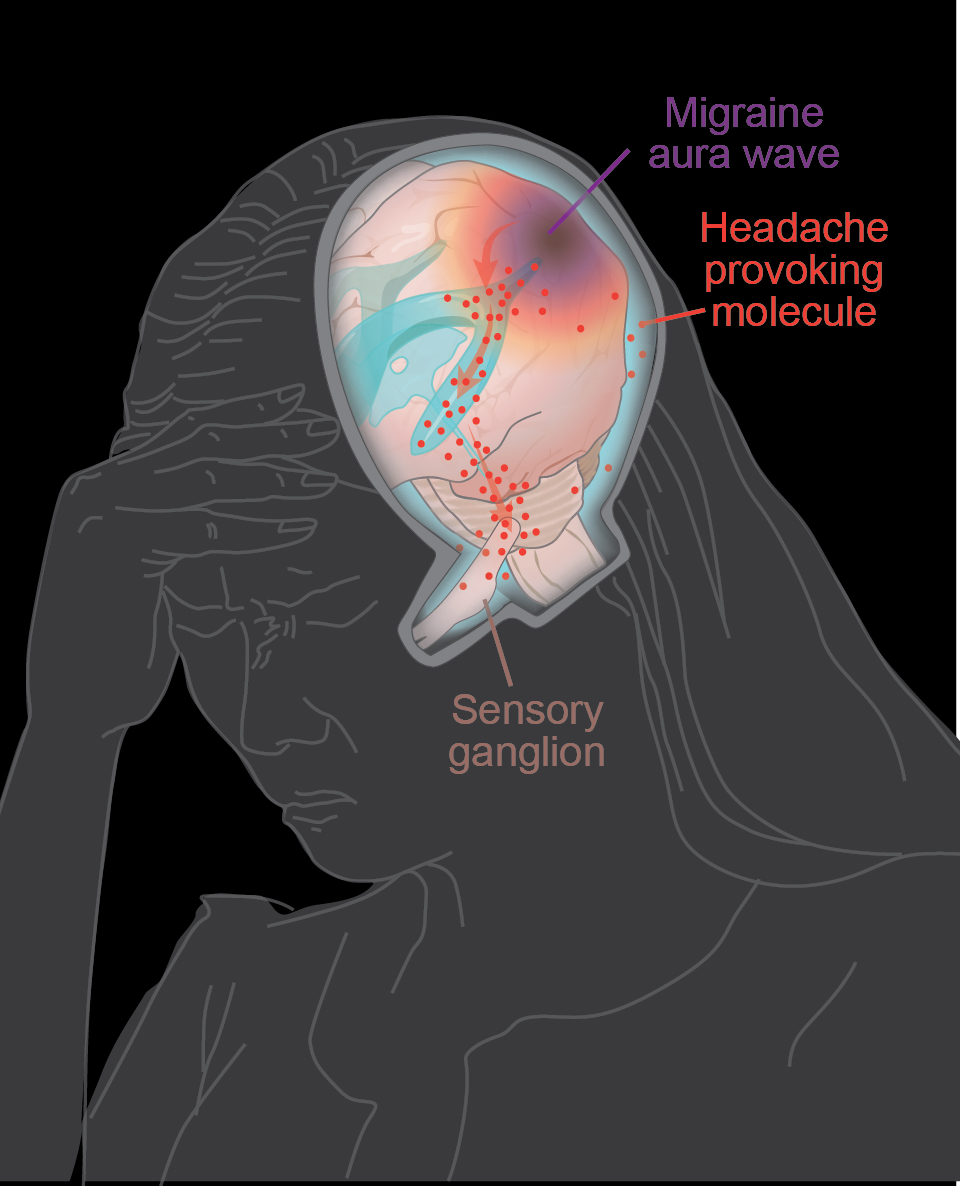
To connect the dots to migraine, the team looked at the effects of cortical spreading depression. They demonstrated that it can increase the flow of CSF in the affected area, carrying more proteins and other molecules to the trigeminal ganglion than it normally would. Many of those proteins were drivers of pain and inflammation.
"We found that during aura, proteins that can activate and sensitize sensory nerves are released to the CSF and transported to the trigeminal ganglion, where they activate pain-mediating sensory nerves," study author Martin Kaag Rasmussen, a postdoctoral scholar at the University of Copenhagen, told Live Science in an email.
"This is what drives the migraine headache, and it is what links the aura phase to the headache," he said.
Related: Does caffeine help or cause headaches?
Of the 12 proteins found to activate pain-sensing nerves, only one — calcitonin gene-related peptide (CGRP) — is a current target for migraine therapies. Medications that block CGRP function relieve migraine symptoms in about half of patients, but that still leaves millions of people without effective treatment.
Rasmussen is optimistic that the additional molecules uncovered in the study could offer new treatment options. "I believe that, when patients do not respond well to currently available therapies, it is because we have not identified what molecule is responsible for their headache," he said.
"I find it really exciting because it's a new pathway for delivery of molecules from the brain to peripheral ganglia," Andrew Russo, a professor of neurology at the University of Iowa who was not involved in the study, told Live Science. That could have relevance well beyond migraines, he said.
The caveat, however, is that all of the group's experiments were performed in mice. In comparison to the human brain, "the mouse brain is very smooth," Russo said. Humans' brain tissue has more folds so the abnormal waves tied to migraine can't travel as efficiently. That might affect how fast CSF flows out of the brain and whether or not it triggers the pain-sensing nerves, Russo noted.
The next step will be to answer that question by examining the same processes in humans or more human-like animal models. The researchers also want to take a closer look at the new pain-triggering proteins they identified, both in migraines and other headache disorders. This could potentially lead to new diagnostic tests and treatments for a variety of patients.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!







