
In our recently published research, our team used machine learning to uncover that hidden information and improve early detection and diagnosis of infection.
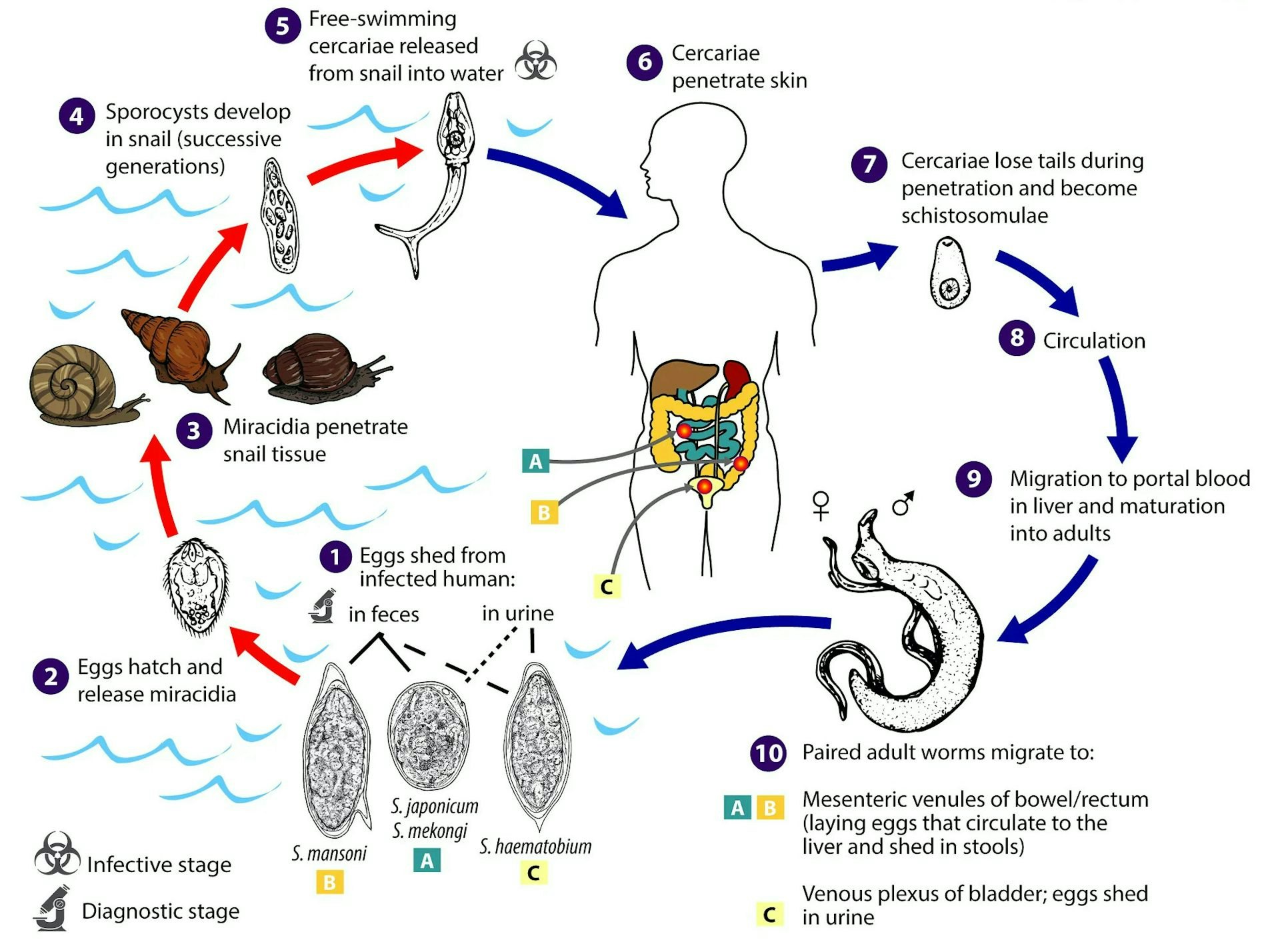
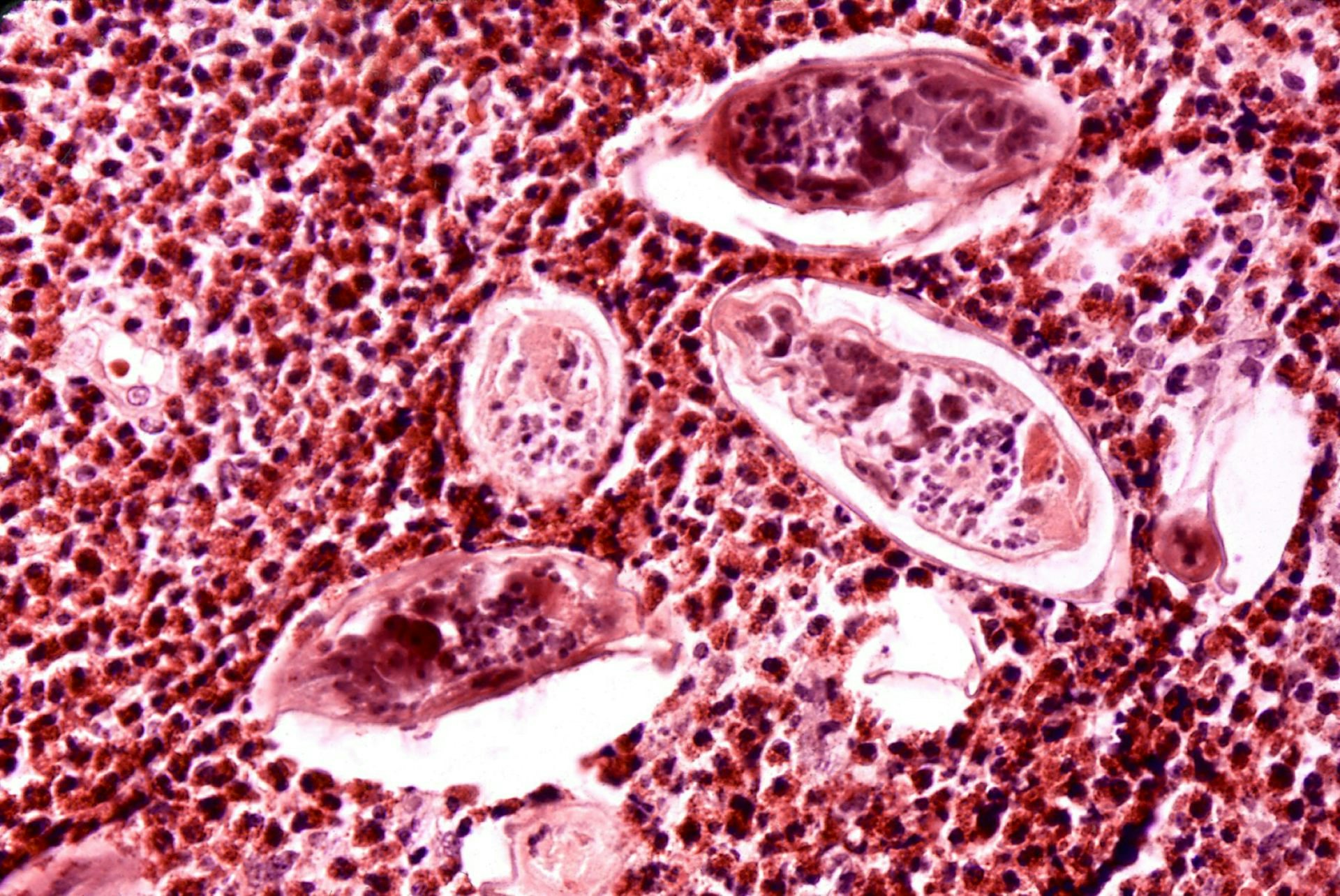
The parasite that causes schistosomiasis completes its life cycle in two hosts — first in snails and then in mammals such as people, dogs, and mice. Freshwater worm eggs enter human hosts through the skin and circulate throughout the body, damaging multiple organs, including the liver, intestine, bladder, and urethra. When these larvae reach blood vessels connecting the intestines to the liver, they mature into adult worms. They then release eggs that are excreted when the infected person defecates, continuing the transmission cycle.
Since diagnosis currently relies on detecting eggs in feces, doctors usually miss the early stages of infection. By the time eggs are detected, patients have already reached an advanced stage of the disease. Because diagnosis rates are poor, public health officials typically mass-administer the drug praziquantel to populations in affected regions. However, praziquantel cannot clear juvenile worms in the early stages of infection, nor can it prevent reinfection.
Our study provides a clear path forward to improving early detection and diagnosis by identifying the hidden information in the blood that signals an active, early-stage infection.
Your body responds to a schistosomiasis infection by mounting an immune response involving several types of immune cells, as well as antibodies specifically targeting molecules secreted by or present on the worm and eggs. Our study introduces two ways to screen for certain characteristics of antibodies that signal early infection.
The first is an assay that captures a quantitative and qualitative profile of immune response, including various classes of antibodies and characteristics that dictate how they communicate with other immune cells. This allowed us to identify specific facets of the immune response that distinguish uninfected patients from patients with early and late-stage disease.
Second, we developed a new machine-learning approach that analyzes antibodies to identify latent characteristics of the immune response linked to disease stage and severity. We trained the model on immune profile data from infected and uninfected patients and tested the model on data that wasn’t used for training and data from a different geographical location. We identified not only biomarkers for the disease but also the potential mechanism that underlies infection.
Why it matters
Schistosomiasis is a neglected tropical disease that affects over 200 million people worldwide, causing 280,000 deaths annually. Early diagnosis can improve treatment effectiveness and prevent severe disease.
In addition, unlike many machine learning methods that are black boxes, our approach is also interpretable. This means it can provide insights into why and how the disease develops beyond simply identifying markers of disease and guiding future strategies for early diagnosis and treatment.
What still isn’t known
The schistosomiasis infection signatures we identified remain stable across two geographical regions across two continents. Future research could explore how well these biomarkers apply to additional populations.
Further, our work identifies a potential mechanism behind disease progression. We found that a particular immune response against a specific protein on the surface of the worm signals an intermediate stage of infection. Understanding how the immune system responds to this understudied antigen could improve diagnosis and treatment.
What’s next
Besides improving our understanding of how the immune system responds to different stages of infection, our findings identify key antigens that could pave the way for designing cost-effective and efficient approaches to diagnosis and treatments. Our next steps will include actually deploying these strategies in the field for early detection and management of disease.
The Research Brief is a short take about interesting academic work.
This article was originally published on The Conversation by Trirupa Chakraborty and Jishnu Das at University of Pittsburgh and Aniruddh Sarkar at Georgia Institute of Technology. Read the original article here.







