The interim results of a randomised phase-3/4 trial carried out in India to evaluate the safety and effectiveness of an all-oral, short-course treatment using just three drugs for people with pre-XDR TB or treatment intolerant/non-responsive MDR pulmonary TB appears promising.
The trial, which has enrolled 400 participants in all, began in October 2021 and is under way at eight sites across the country. The last of the 400 participants was enrolled in end-February 2023. The trial uses just three drugs — bedaquiline, pretomanid and linezolid (BPaL) — and the treatment lasts only for 26 weeks, in contrast to eight-nine tablets each day for 18 months in the case of conventional treatment for drug-resistant TB. While pretomanid and linezolid drugs have to be taken every day for 26 weeks, bedaquiline is to be taken daily for the first fortnight and then every alternate day for 24 weeks.
In all, a person with pre-XDR TB on BPaL regimen will consume over 500 tablets over 26 weeks compared with over 4,300 tablets over 18 months with conventional treatment for drug-resistant TB. The more the number of tablets a day and longer the treatment duration the lower will be the treatment adherence, thus resulting in poor outcomes. This is where the BPaL regimen, which has been approved by the WHO but yet to be implemented in India, becomes superior. India is targeting to reduce TB incidence by 80% and TB deaths by 90% by 2025.
The shorter duration of the BPaL regimen also means that people undergoing the treatment cannot miss even one dose. In short, treatment adherence should be very good.
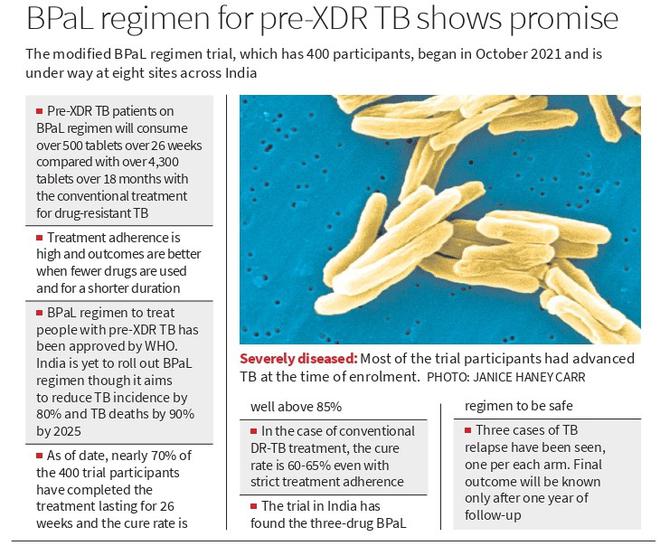
“Nearly 70% of the 400 trial participants have so far completed the treatment lasting for 26 weeks and the cure rate is well above 85%,” says Dr. C Padmapriyadarsini, Director of the Chennai-based National Institute for Research in Tuberculosis (NIRT) and the trial coordinator. “In the case of the conventional treatment for DR-TB, the cure rate is 60-65% even when patients strictly adhere to the treatment regimen.”
“Most of the patients who have been enrolled in the trial had advanced TB at the time of enrolment. They had extensive disease affecting both their lungs. Yet, the cure rate has been over 85%. This establishes the superiority of the BPaL short-course therapy,” she says. “The outcomes will become even better if pre-XDR patients are diagnosed early and put on treatment with the three-drug regimen.”
According to Dr. Padmapriyadarsini, the three drugs have been found to be safe. “Serious adverse effects were seen in three-four trial participants, which were either managed or were too late stage of the disease to be helped. This makes it important to get diagnosed early and treatment initiated immediately,” she says. “There were a few cases of mild adverse effects caused by linezolid such as a drop in haemoglobin and platelet counts, and neuropathy such as tingling sensation and numbness in the legs.” According to her, anaemia caused by linezolid was seen in 10-15% of trial participants. Intervention to address anaemia was started when there was 10% reduction in haemoglobin count. Neuropathy was seen in a few trial participants.
“Since we have been closely monitoring the participants, we were able to capture anaemia early and intervene immediately. We had to change the treatment and use a different regimen in a few participants due to adverse effects,” says Dr. Padmapriyadarsini. The participants were monitored every 15 days all through 26 weeks of treatment. The follow-up will continue for a year after the end of 26 weeks of treatment.
All these adverse effects— a drop in haemoglobin count and platelets, and neuropathy — were seen only in the first two months of treatment when 600 mg linezolid was used per day. The adverse effects were resolved when the dosage of linezolid was reduced to 300 mg, she says. A study done earlier by Dr. Padmapriyadarsini and her team found that more trial participants had neuropathy after three-four months of treatment with linezolid, and this was resolved when the linezolid dosage was halved to 300 mg per day. Results of that trial served as a basis for using 600 mg of linezolid only for 13 and nine weeks in the two intervention arms and reducing the dosage to 300 mg for the rest of the treatment duration in the current trial.
Since linezolid causes a drop in haemoglobin count and neuropathy, the trial is testing two regimens using lower doses of linezolid. In all, the trial has three arms with over 100 participants each. Participants in the control arm were given the WHO-approved BPaL regimen of 600 mg linezolid for 26 weeks. In one intervention arm, the participants were given 600 mg of linezolid daily for 13 weeks followed by 300 mg of linezolid for the remaining 13 weeks. In the second intervention arm, the participants were given 600 mg of linezolid daily for nine weeks followed by 300 mg of linezolid for the remaining 17 weeks.
The primary outcome of the current trial is to evaluate sustained treatment success at the end of one year post TB treatment using the BPaL regimen. Three cases of TB relapse have been seen, one per each arm. Since follow-up will continue for 12 months after 26 weeks of treatment, the final outcome will be known only after a year.







