
Systems and processes in place around patient safety failed in terms of the work of a Belfast-based neurologist, an inquiry has found.
Dr Cathy Jack, chief executive of the Belfast Health Trust, has apologised to Dr Michael Watt’s former patients, saying the trust let them down.
She said she would not be resigning, saying she did not believe this “incredibly difficult time” for the health service and trust would be improved if leaders “abandon their posts”.
“I have important work to do in very difficult circumstances in order to build safer and better services for patients, service users and staff, and I intend to get on with doing it,” she said.
Dr Watt was at the centre of Northern Ireland’s largest ever recall of patients, which began in 2018, after concerns were raised about his clinical work.
More than 4,000 of his former patients attended recall appointments.
Almost a fifth of patients who attended recall appointments were found to have received an “insecure diagnosis”.
While one process or system failure may not be critical, the synergistic effect of numerous failures ensured that a problem with an individual doctor's practice was missed for many years.— Independent Neurology Inquiry report
The final report following the Independent Neurology Inquiry found that problems with Dr Watt’s practice were missed for years and opportunities to intervene were lost.
It makes 76 recommendations to the Department of Health, healthcare organisations, General Medical Council and the independent sector.
“While one process or system failure may not be critical, the synergistic effect of numerous failures ensured that a problem with an individual doctor’s practice was missed for many years and, as this inquiry finds, opportunities to intervene, particularly in 2006/2007, 2012/2013, and earlier in 2016 were lost,” the inquiry found.
The inquiry, led by Brett Lockhart QC, examined whether there were complaints or concerns which should have alerted the Belfast Health Trust to instigate an earlier investigation.
It concluded that the trust could and should have intervened earlier but failed to do so.
However the report also finds the failings identified were not confined to the trust.
“The inquiry has concluded that the combined effect of an inadequate investigation into a highly relevant clinical complaint in 2012 by the regulator (the General Medical Council); the failure to disclose significant complaints by the Ulster Independent Clinic, where Dr Watt had a substantial private practice; alongside failures of other HSC trusts to identify a pattern of concern was a conspicuous problem in the Belfast Trust,” the report finds.
“Generally, the inability of the systems then in place to identify a pattern of concern was a conspicuous problem.
“Information was essentially retained in silos.
“Communication between different organisations and between management levels within organisations was poor and inadequate.”
Patients will, however, rightly point to the many years when problems that emerged with Dr Watt were not addressed, opportunities were missed and such inaction was to the significant detriment of patients— Independent Neurology Inquiry report
The report also found that while not every step taken after November 2016 was correct, the inquiry panel believes the Belfast Trust got key decisions right after that date.
Those included the partial restriction of Dr Watt in December 2016, the commissioning of a report into his practice by the Royal College of Physicians, the full restriction of his practice in July 2017 and the decision to initiate a large-scale patient recall in May 2018.
“Patients will, however, rightly point to the many years when problems that emerged with Dr Watt were not addressed, opportunities were missed and such inaction was to the significant detriment of patients,” the report added.
Mr Lockhart described the report as “fundamental about the safety of patients”.
“Would earlier interventions have made a difference, the inquiry panel believes that it would have done,” he said.
“The inquiry panel has concluded that the Belfast Trust could and should have intervened earlier but failed to do so over many years.”
He described the probe as one of a number of inquiries and reports into the health service.

“Accountability is rightly sought by the public and especially patients who have suffered harm,” he said.
“Indignation at failings is a justifiable response but what is urgently required is reform, change and implementation.
“A key theme of the recommendations is ensuring the disclosure and investigation of information for the enhancement of patient safety.
“The onus is now on everyone involved in the delivery of healthcare from the political representatives to the Department of Health and the Health Trusts, from the regulator to the independent sector, to ensure the recommendations of this report are properly considered and implemented.
“The goal is a healthcare system which makes patient safety its paramount concern whatever the question being asked, or the issue determined. Patients who have waited for so many years deserve nothing less.”
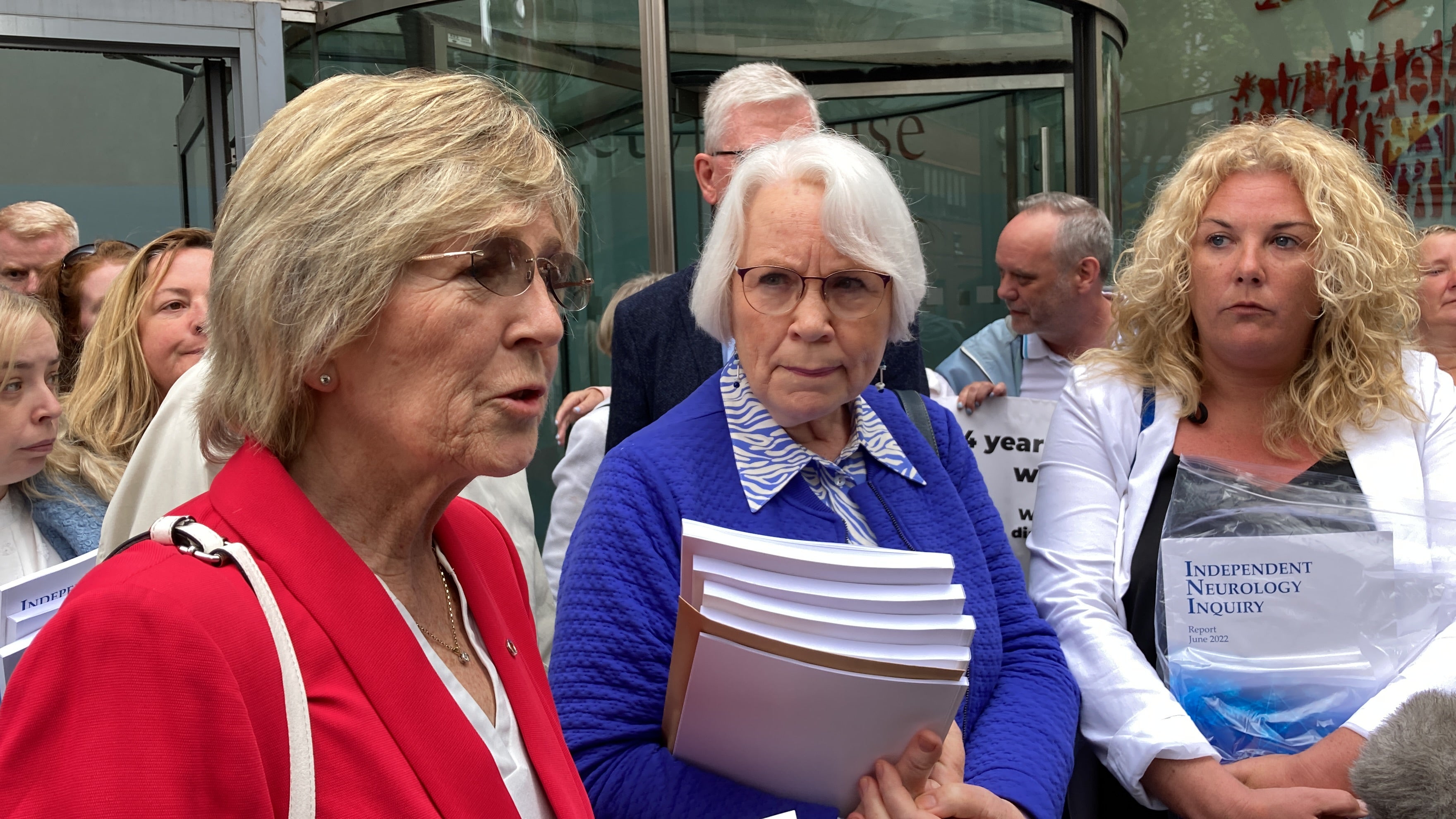
Danielle O’Neill, a former patient of Dr Michael Watt, was among those who attended the unveiling of the report.
“Michael Watt failed us, the Belfast Trust failed us, the department of health failed us, the GMC failed every single patient caught up in this scandal,” she said.
“They should all do the honourable thing, hang their heads in shame and resign.”
Almost a fifth of patients who attended recall appointments amid concerns about the work of a Belfast-based neurologist received an “insecure diagnosis”, a final outcomes report undertaken by the Department of Health and published earlier in June found.

Health Minister Robin Swann apologised unreservedly for the hurt caused.
A number of separate inquiries have been taking place into the work of Dr Watt, who formerly worked for Belfast Trust at the Royal Victoria Hospital.
Last year, he was allowed to voluntarily leave the medical register before a General Medical Council hearing could be carried out into his actions.
This means he can no longer practice medicine in the UK.







