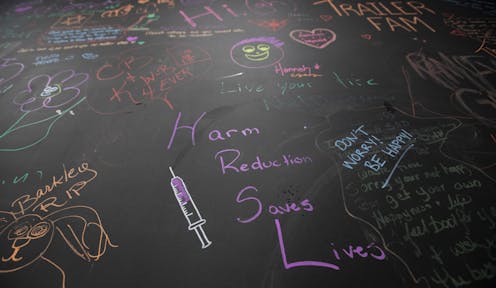
Since 2016, more than 32,000 Canadians have died from drug overdoses. In response to this overdose epidemic, several provinces have established Supervised Consumption Sites (SCS), which provide people who use drugs with a safe space to administer drugs under the supervision of trained staff.
The term people who use drugs is used to affirm people’s humanity instead of defining them by their drug use. Person-centred language helps reduce stigma and discrimination which in turn can encourage people who use drugs to seek out harm reduction services.
SCSs have proven to reduce drug overdoses, disease transmission and public drug use. By 2020, there were 39 supervised consumption sites across Canada. Yet despite the evidence, some governments continue to oppose safe consumption on ideological grounds.

Alberta is a prime example of how policy shifts away from public health approaches have tangible effects for the well-being of people who use drugs. Our research with marginalized drug users in Lethbridge, Alta. demonstrates that the closure of SCSs can increase drug-related harms and negatively impact the safety and welfare of people who use drugs.
Lethbridge’s SCS
Prior to the province approving a supervised consumption site in Lethbridge, the city had long contended with high numbers of drug overdoses. Opened in 2018, Lethbridge’s site quickly became the busiest in North America. This was in part because it offered a range of crucial social, mental and health service resources to marginalized community members.
But the site’s success was short-lived. The provincial government defunded and replaced it with an Overdose Prevention Site (OPS) just two years later. The OPS, while well intentioned, provides limited social, mental and health resources as compared to the SCS.
Moreover, while the former SCS was in the city’s downtown core, the new overdose prevention site was placed in an industrial area, about a 10-minute walk away from where many local people who use drugs spend time. Those interviewed as part of our research experienced this new location as less safe.
In Lethbridge, the SCS’s closure and replacement with an overdose prevention site meant reduced access to harm reduction services. In addition, the site’s closure stripped local people who use drugs of access to essential community connections and services.
Most people we spoke with felt overdoses and drug-related deaths had increased because of the SCS’s closure, with many having lost loved ones. As one of the participants told us: “There’s too many people dying now.”
Supporting participants’ views, provincial health data demonstrates that the average number of deaths from drug poisoning doubled in Lethbridge following the site’s dismantling.
If the goal is to extend harm reduction services to as many people as possible, it is imperative to illuminate what prevents some people who use drugs from routinely accessing the OPS.

How policy change can affect people who use drugs
In spring 2022, we spent time in downtown Lethbridge, getting to know those who identified as people who use drugs and expressed interest in talking to us. We interviewed 50 houseless people, asking them about their experiences of street life in Lethbridge, whether or not they access the new OPS and why.
Our research provides early evidence that recent provincial policy shifts have negatively impacted people who use drugs in Lethbridge. The majority of those we spoke with who routinely accessed the SCS prior to its closure chose not to access the new OPS.
Participants listed several barriers to accessing the overdose prevention site.
First, the new site does not have a supervised smoking room. This means that those who smoke illicit substances, or who want to replace safe injection with safe smoking, cannot do so in the facility. This is further concerning because, while smoking drugs carries a number of risks, smoking instead of injecting drugs can decrease skin infections and exposure to blood-borne viruses.
Second, many participants stated that they were fearful of accessing the OPS and spending time in the area. To get from the downtown core to the OPS, they must cross a high-traffic bridge where participants stated people driving by sometimes harass or assault them. There have also been reported concerns over conflict and violence in the vicinity of the overdose prevention site. Accordingly, some people who use drugs often avoided the OPS, opting to consume in “safer,” usually public, areas.
Finally, people who use drugs reported that they often frequented the old SCS because it offered them with wraparound services, social connections and activities beyond supervised consumption. But the OPS lacks these diverse and critical benefits. Because of this, participants felt the OPS was not as responsive to their broader needs.
Undeniably, Lethbridge’s overdose prevention site is providing important health benefits. However, our findings suggest that harm reduction sites that provide marginalized community members with broad community services and connections are more likely to draw local people who use drugs in, encourage uptake and reduce drug-related harms.
Given Lethbridge’s continued challenges with drug-related harms and deaths, it is essential to build safe, accessible and comprehensive harm reduction resources that provide critical care to the city’s most marginalized.
Carolyn Greene receives funding from the Social Sciences and Humanities Research Council.
Katharina Maier receives funding from the Social Sciences and Humanities Research Council.
Marta-Marika Urbanik receives funding from the Social Sciences and Humanities Research Council and Killam Trusts.
This article was originally published on The Conversation. Read the original article.







