Scientists have found that a special fluid linked with immunity in the brain can reach the skull’s bone marrow via tiny channels that help in the detection and response to infection or injury.
The findings, published in the journal Nature Neuroscience last week, may have “huge implications” for conditions like dementia and Alzheimer’s disease since these diseases have an inflammatory component, researchers say.
Scientists, including those from Massachusetts General Hospital (MGH) in the US, believe the findings also shed more light on how immune cells produced in the spongy tissue of the skull’s bone marrow can screen the brain’s cerebrospinal fluid (CSF) for signs of infection and other threats to the brain.
Previous studies have shown that interactions between the body’s immune and central nervous systems strongly influence brain health.
Although the blood–brain barrier restricts crosstalk between these two systems and prevents the entry of harmful pathogens into the brain via the blood, research has shown that special gateways through this brain border exist that facilitate intersystem communication and regulate brain health.
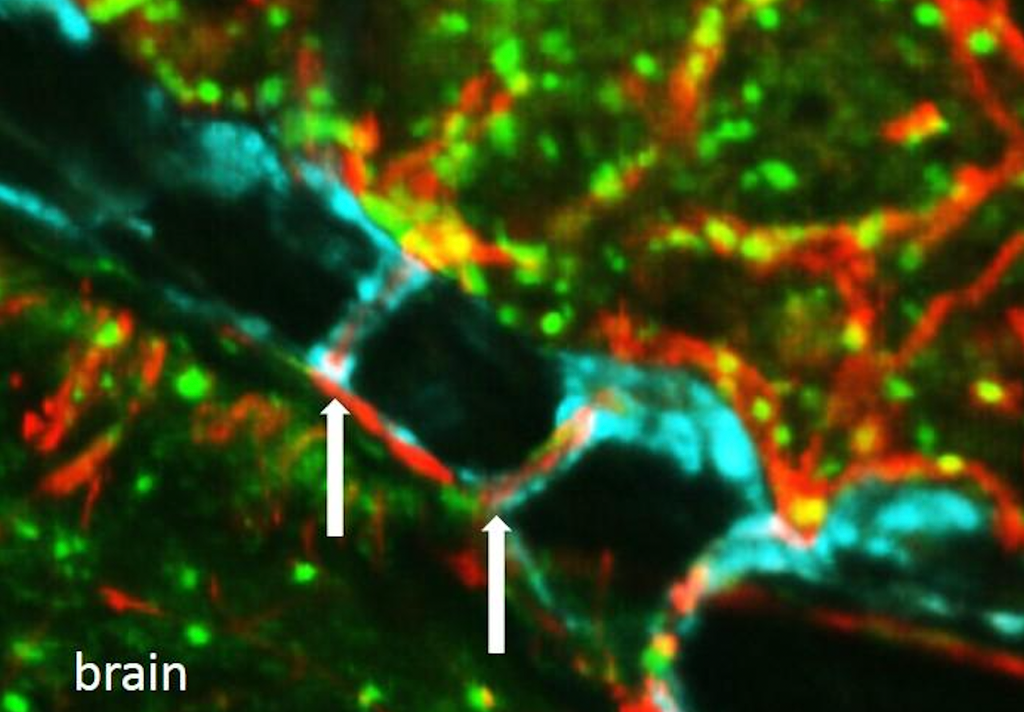
In an earlier study in mice in 2018, researchers had found that immune cells responding to brain infection and injury come from bone marrow in the skull, passing through hundreds of tiny, previously unknown channels.
These connect the skull’s bone marrow to the outer layers of membranes that cover the brain called meninges.
In the new research, scientists have found that in addition to allowing immune cells to flow from the skull’s bone marrow to the meninges, these tiny channels in the skull also allow the cerebrospinal fluid to flow in the opposite direction – out of the brain and into the skull’s bone marrow.
“Now we know that the brain can signal to this hub of immunity — in other words, cry for help in case things go wrong, such as during infection and inflammation,” study co-author Matthias Nahrendorf said in a statement. “Cells in the skull’s bone marrow are surveilling the cerebrospinal fluid that exits the brain through the skull channels we discovered earlier.”
Researchers also found that bacteria inflammation of the meninges (meningitis) travel through the channels and enter the skull’s bone marrow, causing cells in the bone marrow to produce more immune cells like leukocytes to combat the invasion.
“As skull channels also directly provide leukocytes to meninges, the privileged sampling of brain-derived danger signals in CSF by regional marrow may have broad implications for inflammatory neurological disorders,” the scientists wrote.
The findings, they believe, could also lead to new strategies to treat such bacterial meningitis which causes around 250,000 deaths a year across the globe.
“Our work may also be helpful for studying situations when the immune response is harmful, such as when skull bone marrow–derived immune cells damage the brain and surrounding nerves,” Nahrendorf said.
“Understanding what fuels neuro-inflammation is the first step to successfully modulating it,” he added.







