
The population aged 75-plus is set to triple in the next 50 years, but aged care providers say they’re short 1000 nurses and it’s only getting worse
Retirement village firm Summerset reveals that at the peaks of the Covid outbreaks the 2100-strong company diverted head office and sales staff to work with residents in the retirement homes, but it wasn't enough.
The company is building villages faster than any other operator, with consents for villages at Prebbleton, Rangiora, Blenheim, Cambridge, Waikanae and Milldale. It's seeking to fast-track approval for a Half Moon Bay retirement village in east Auckland, and plans another in Palmerston North.
With five sites in Australia as well, those will bring the number of Summerset villages to 46. But it can't staff them.
NZ Aged Care Association surveys show there are close to 1,000 vacant positions for registered nurses across the aged care industry. It's a concern echoed by other retirement village providers such as Arvida and Oceania, calling it a "workforce crisis". Forty-eight percent of the registered nurses in the sector left their jobs last year, Summerset said.
Summerset's new chief executive Scott Scoullar told shareholders yesterday at the company's annual meeting that finding nursing staff had been an ongoing issue for the sector this year. "Increases to public sector nursing wages and immigration constraints induced by Covid have created a perfect storm for nursing shortages in aged care."
"We will not compromise our standards, but there are many operators across the sector who are looking at having to close their doors for good." – Scott Scoullar, Summerset
The company had increased nurses' pay rates to remain competitive with the public sector, but management were "very concerned" about under-funding in the aged care sector.
"Overall public funding for care services, including daily care rates, is insufficient to provide the exacting standards of service that are rightly expected," Scoullar said.
He said the Government funded aged care nurses nearly $20,000 a year less than in public hospitals. Despite this, the company had invested an additional $4.3 million in new roles or additional care wages in 2021.
"We also acknowledged that alert level 4 placed extra stress on our frontline staff, and we paid our village and care staff a sector-leading $3 extra per hour during that period, reflecting the high value we place on the work of our employees.

"We will not compromise our standards, but there are many operators across the sector who are looking at having to close their doors for good."
The aged care sector across New Zealand has nearly 40,000 beds, compared with public hospitals' 14,000 beds. He warned that if action wasn’t taken by the Crown to fix the underfunding for the sector, this would have "a large detrimental impact on New Zealand’s public health system".
Summerset chair Mark Verbiest told the meeting the company had increased nurses' pay rates to keep up with the public sector last year, to attract and retain the vital nursing staff it needed to care for elderly residents. But, he reiterated, the company was concerned about underfunding in the aged care sector.
"Admissions at some care centres have occasionally paused to manage staffing levels." – Jeremy Nicholls, Arvida
"Overall public funding for care services, including daily care rates, is insufficient to provide the exacting standards of service that are rightly expected," he said. "Frontline and care staffing and remuneration is a serious issue for the whole sector and for New Zealand."
The Aged Care Association has made a submission to the Productivity Commission's immigration inquiry, saying registered nurses' wages in aged residential care are restricted by the funding model.
And turnover rates are high as nurses quit the sector because of the stresses of staff shortages, meaning there will be a continued reliance on migrant nurses until tertiary institutions provide more places for nurse training.
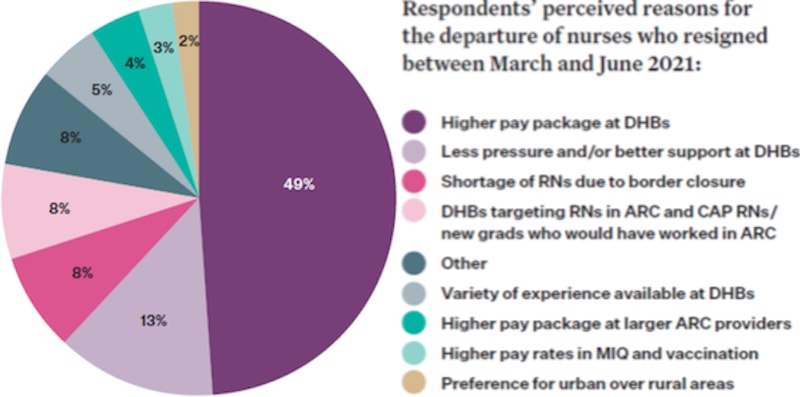
As this chart shows, half the departing nurses are bound for district health boards where they can get better pay. Others are going to bigger retirement villages or to vaccination centres, again because they pay better.
Other retirement village providers have also highlighted the impact on staffing.
In Oceania's interim report, chair Elizabeth Coutts called it a "workforce crisis", exacerbated by the impact of the Covid-19 border restrictions on arrivals of registered nurses from overseas. The company was providing additional professional development, improved employee benefits and reviewing pay, in a bid to stem the exodus.
Ryman Healthcare group chief financial officer David Bennett told investors in November the company had spent an additional $7.6m on staffing, security, and resident welfare during Covid. "The New Zealand Government's decision to give many of our workers a pathway to residency was fantastic news," he said. "They've worked tirelessly with dedication and loyalty throughout the Covid crisis."
And Arvida chief executive Jeremy Nicoll, in a newsletter to investors this month, said Omicron and the traffic light settings had required additional investment in people, PPE and rapid antigen tests of about $4m-$5m. That included an hourly bonus for staff during phase 3 of the Government’s red traffic light setting. "Admissions at some care centres have occasionally paused to manage staffing levels," he said. "This has meant care occupancy has tracked lower over the fourth quarter."
As well as affecting nursing staff, lockdowns and isolation had affected construction workers and slowed progress on Arvida's building projects.







