As Aotearoa New Zealand heads into the colder winter months, the pressures on our health system and staff are growing significantly.
On top of the ongoing impact of COVID-19, flu cases have begun to spike.
Conditions are also primed for potential outbreaks of other illnesses including measles, whooping cough and respiratory syncytial virus (RSV).
If we are to weather the coming storm, there will need to be a recommitment to public health measures that slow the spread of respiratory infections, as well as a renewed drive for widespread vaccination.
The first wave of Omicron swept through Aotearoa New Zealand in late February and March.
Unfortunately, as seen in many other countries, the fall in case numbers has been much slower than the rise, with infections reaching a plateau in all age groups.
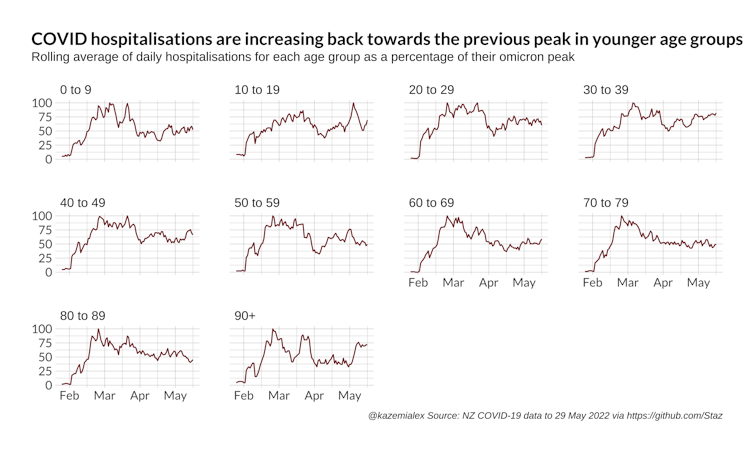
Case numbers have been driven by a high number of infections in young people between the ages of 10 and 29 years old. But the elderly have borne the brunt of hospitalisations, largely due to the higher risk of severe outcomes for older adults.
Age stratification aside, persistent inequities have also left Māori and Pasifika at the sharp end of the outbreak both in terms of cases and severe outcomes.
Hospitalisation rates and reinfections are rising in many age groups, mirroring trends seen elsewhere.
An unwanted COVID-19 resurgence
New Zealand can expect another resurgence of COVID-19 this winter.
While 95% of New Zealand has received the second dose of the vaccine, one of the highest rates in the world, fewer have received a booster. We also have lower than optimal levels of childhood vaccination.
Long COVID will add a layer of complication for our medical services.
A recent report by the US Center for Disease Control (CDC) suggests one in five COVID-19 survivors aged 18 to 64 years old, and one in four survivors aged 65 years and above, experienced at least one condition that might be attributable to previous COVID-19 infection.
Despite being labelled as one of this generation’s disability challenges, there is currently no test for long COVID.
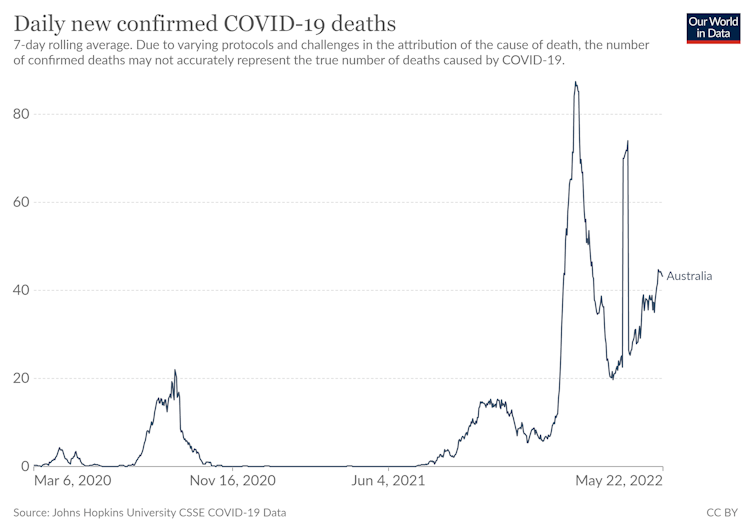
Worryingly, COVID-19 deaths in Australia have started to trend upwards. Evidence from Australia has shown that the overwhelming majority of people are dying from, not with, COVID-19.
Winter will bring more than COVID-19
Health professionals are not just worried about COVID-19. The flu and other viruses are also expected to hit hard this year.
Thanks to closed borders, managed isolation and quarantine, and lockdowns, the last time New Zealand experienced a flu season was in 2019.
We are now more vulnerable to the virus. There has already been a reported surge in Dunedin.
In response, the government has made two million vaccines available and has the widened eligibility for people to get vaccinated for free.
Unfortunately, there is growing concern that part of the population may not get vaccinated due to immunisation fatigue, or may be unable to due to structural inequities in access to vaccines.
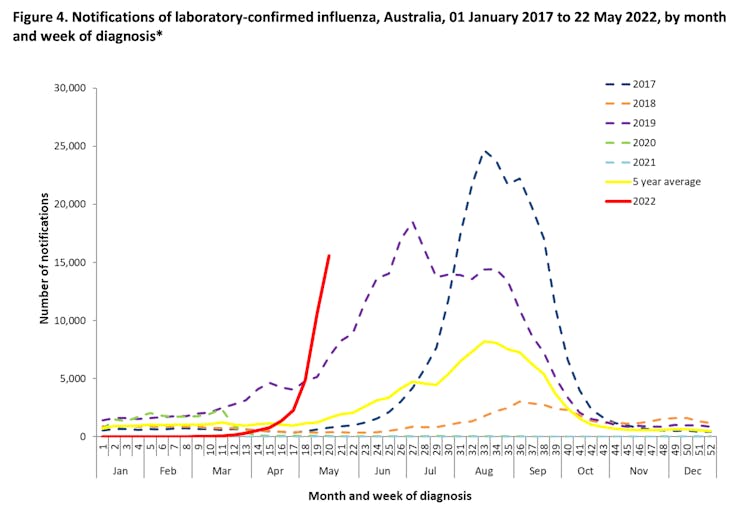
As with COVID-19, looking across the Tasman can help us understand what is likely to happen in New Zealand.
Much like New Zealand, flu rates in Australia have, until now, been very low due to closed borders.
The latest Australian national surveillance for influenza shows a steep rise in rates of the flu, as well as rising hospital and ICU admissions.
Vaccination gaps exist for other diseases
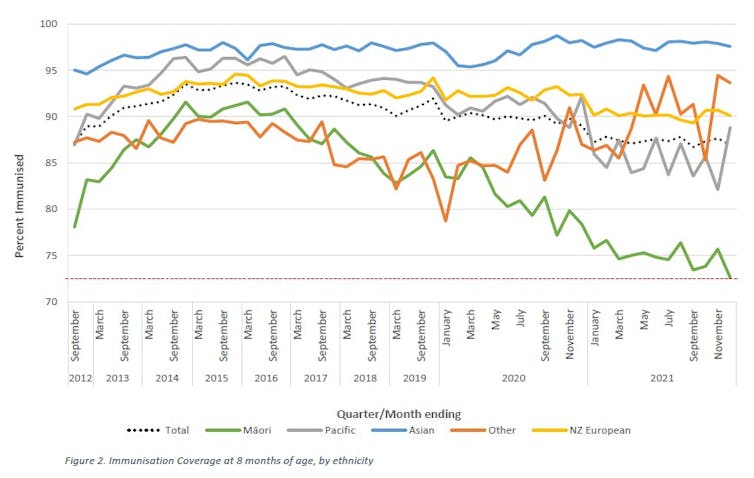
Before the COVID-19 pandemic even started, our research highlighted declines in childhood immunisation for vaccine-preventable diseases.
Public health officials are now noticing further significant declines in routine childhood immunisations.
In April, the World Health Organization reported a 79% increase in measles cases in the first two months of 2022.
Meaningfully addressing long-standing inequities in childhood vaccination programmes takes on new urgency in the face of these vaccination gaps.
Lessons can also be learned from the COVID-19 vaccination programme regarding the success of handing leadership to Māori and Pasifika community providers to improve vaccination rates.
The health system is under unprecedented pressure
We have long been warned that an underfunded health system might struggle with a seasonal surge in demand.
Pressure points have appeared across the country. On May 23, Dunedin Hospital’s COVID-19 ward was at capacity. Two days later, Nelson Hospital also hit capacity limits, leading to temporary ambulance ramping at the emergency department.
Canterbury District Health Board, Hawke’s Bay District Health Board, and MidCentral District Health Board have recently urged people to consider alternative care for minor conditions to help alleviate the pressure.
Community health providers are also struggling to meet demands.
What can you do?
During the winter, we spend more time in indoor spaces with inadequate ventilation. We are also becoming more complacent with our mask wearing as policies relax.
In the future, vaccines will need to improve.
But for now, it’s important to remember that three doses of the COVID-19 vaccine remain effective against hospitalisation even for newer variants, as well as lowering the risk of infection.
But there are things we can all do to avoid the worst this winter has to offer, including to:
- ventilate indoor spaces – especially in crowded rooms
- wear appropriate masks where social distancing is not possible, particularly indoors
- get vaccinated against COVID-19, which helps to protect you from the most severe form of COVID-19, as well as protecting others by decreasing transmission. Other routine vaccinations for flu and measles will also be important to consider.
Finally, workplaces should continue to support people to stay home and isolate if required.
Dr. Matthew Hobbs receives funding from the New Zealand Health Research Council, Cure Kids/A Better Start National Science Challenge and IStar. He was also previously funded as a researcher by the New Zealand Ministry of Health.
Lukas Marek has previously received funding from the Ministry of Health, New Zealand Health Research Council, Cure Kids and National Science Challenges.
Alex Kazemi does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
This article was originally published on The Conversation. Read the original article.