
Brain stimulation that rapidly adjusts in real-time can dramatically reduce Parkinson's symptoms, a small, early trial suggests.
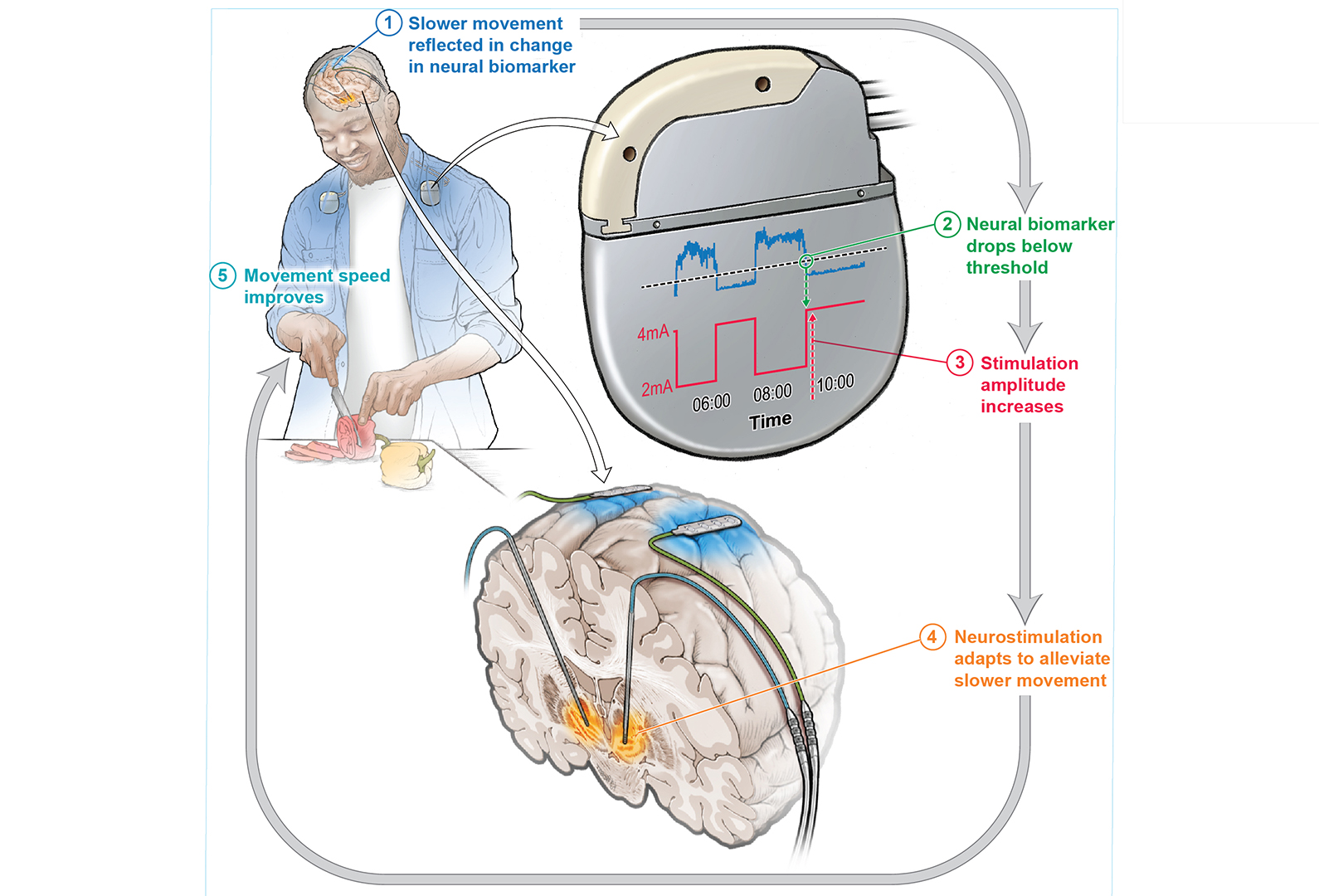
The device in question, described in a paper published Monday (Aug. 19) in the journal Nature Medicine, uses implanted electrodes that automatically respond to brain signals associated with slow movement or spasms seen in Parkinson's patients. The device then gives more or less electrical stimulation as needed.
By comparison, traditional brain stimulation delivers constant electrical stimulation and patients must have the degree of stimulation adjusted by a doctor.
The new adaptive deep brain stimulation (aDBS) system "cuts the duration of their motor symptoms in half and increases their quality of life," lead study author Dr. Carina Oehrn, a cognitive neuroscientist at the University of California, San Francisco, told Live Science.
Related: New blood test could flag Parkinson's disease years before symptoms, study hints
Parkinson's disease is a neurodegenerative disease in which specific brain cells that make dopamine malfunction and steadily die off. These cells play a critical role in movement.
Most Parkinson's patients take levodopa, a drug that elevates dopamine levels in the brain. But as the disease progresses, levodopa often stops being enough to manage the symptoms.
At that point, many patients complement the drug with constant deep brain stimulation (cDBS), in which surgeons implant electrodes that alter the signals underpinning Parkinson's symptoms. While the treatment is safe and works, because the stimulation is constant, it can both under- or over-compensate for a person's symptoms.
To see if there could be a better approach, Oehrn and colleagues implanted a device that could switch between providing continuous or aDBS in four men with Parkinson's disease. The researchers asked each patient which symptom bothered them most; three said bradykinesia, or slow movement, while the last said spasms. Then they zeroed in on the brain signal related to the problem symptom.
After continuously recording from two brain regions, the team trained algorithms to predict the course of a patient's symptoms and respond to them. The aDBS device reacted to a brain signal that marked when a patient's dopamine levels rose — right after they took their medication — and fell as the effects of the drugs wore off.
After the training period, the patients, some of whom work full time, left the clinic and went about their daily lives. The device then delivered either cDBS or aDBS, switching back and forth over time. In theory, patients didn't know which type of stimulation was active at any given time.
"But after a while, they could really tell the days when they were on aDBS just because their motor symptoms were controlled so well," Oehrn said. The patients rated which stimulation they preferred through a phone app, reporting aDBS to be superior.
Oehrn said there are likely many patients for whom cDBS alone will suffice because their symptoms don't change throughout the day. Those whose symptoms fluctuate would be most likely to benefit from the new system, she suggested.
While the researchers focused on just one type of symptom at a time for this study, Oehrn hopes future algorithms can respond to additional symptoms. Next month, they will see how the device affects the memory and mood problems tied to Parkinson's, Oehrn said.
The study is noteworthy because it looked at a new type of brain signal as a trigger for activating the device, which could open the door to a wider range of applications than has previously been considered, Dr. Martijn Beudel, a neurology specialist at the Amsterdam University Medical Center, told Live Science in an email.
The new research has "significantly advanced" the therapy's potential in treating Parkinson's disease, said Beudel, who was not involved in the study.
This article is for informational purposes only and is not meant to offer medical advice.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!
.jpg?w=600)






