Why are babies born prematurely? Researchers still don’t really know.
Obstetricians are very good at managing the process of birth. But when it comes to predicting whether a baby will be born in a timely manner, the science is still catching up. Research on the causes of preterm birth is decades behind that of other conditions such as cancer. That means nurses, doctors, midwives and doulas don’t have the tools and resources they need to do the best job possible when babies are born before 37 weeks of pregnancy.
One of the few known risk factors of preterm birth is whether a pregnant person has previously given birth to a preterm baby. Others include being pregnant with twins, triplets or more, and certain medical conditions such as urinary tract infections, high blood pressure or diabetes. Knowing these risk factors, however, does not always pinpoint the cause of preterm birth.
Progress has been slow in part because much of the research to date on preterm birth has approached pregnancy from the perspective of reproductive biology. That includes the enormous physiological changes across the reproductive, cardiovascular and endocrine systems of the pregnant person, and the influence of hormones and genetics on both parent and fetus.
Yet pregnancy is also an engineering challenge because it involves physical forces. Clinicians are dealing with an average 7-pound (3.2 kg) baby in around 1 liter of amniotic fluid held in place with a membrane less than 1 millimeter thick – all within a uterus that started out the size of a fist. That involves forces, pressures and mechanical loads that all can contribute to maternal, fetal and placental conditions that can trigger preterm birth.
In a paper published over 150 years ago, a physician recognized that birth is a mechanical event. But he was using 19th-century technology to measure the pressure per area on membranes that support pregnancy. Only now do researchers have the mechanical, electrical and computational engineering expertise to address the challenges of preterm birth.
But research on preterm birth is still so early that scientists first must build the tools to study it before they can diagnose and treat it. Our team of researchers is working to do just that.
Many complications can cause preterm birth
It’s hard to narrow down who is at risk of preterm birth because there is no single cause. Preterm birth can be triggered by multiple factors involving the pregnant person, the fetus, the placenta or the fetal membranes attached to the placenta that connect fetus and parent.
Globally, 1 in 10 live births are preterm, or born before 37 weeks of pregnancy. Of these preterm births, about 30% to 40% are caused by premature rupture of the fetal membranes, and another 1% to 9% by the cervix dilating prematurely.
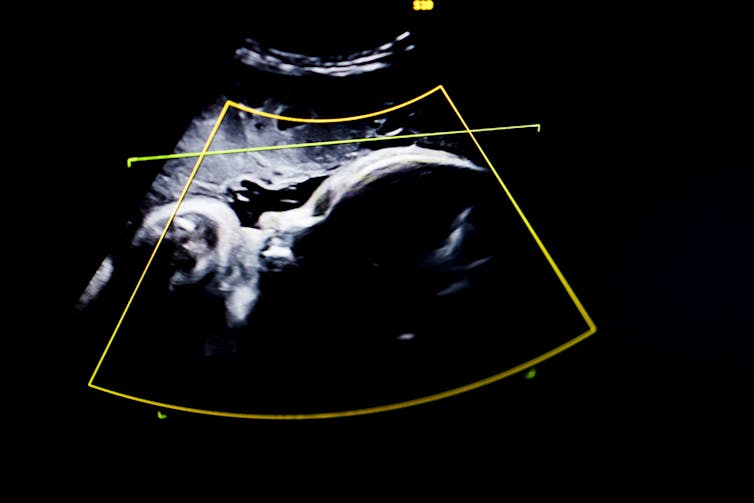
With current technology, preterm births are rarely preventable. Current screening tools to measure the risk of preterm birth are fairly primitive. Doctors use ultrasound to monitor the size and position of the baby, and they touch the cervix to feel whether it is softening, a normal process prior to labor but problematic if it is happening too soon.
If the baby isn’t growing, perhaps because of insufficient blood supply to the placenta, doctors perform preterm C-sections to prevent stillbirth. Preemptive C-sections are also sometimes used to prevent or treat preeclampsia, or dangerously high blood pressure during pregnancy.
In both cases, patients and doctors balance the benefit of an early C-section for the fetus and the parent against the risks associated with preterm birth, including a lifetime of breathing, vision, cardiovascular or other health issues for the child.
The wide variety of factors that play a role in preterm birth make early diagnosis a challenge. But a better core understanding of the biomechanical forces at work during pregnancy can give researchers new places to look for diagnostic clues.
Tackling the challenge from multiple angles
Pregnancy is essentially a physical process, from the uterus stretching to accommodate the baby to the cervix dilating when labor contractions begin and it’s time for the parent to push. And when something mechanical goes wrong, it can lead to tragic results.
For example, maternal risk factors for preterm birth include rupture of the uterus or preeclampsia. The placenta could also detach from the wall of the uterus, causing the parent to bleed to death. Carrying twins comes with additional amniotic fluid and blood volume that adds an extra load to the placenta, which can trigger preterm labor.
Our team of biomechanical and biomedical engineers is working to understand the underlying causes of preterm birth from different angles, all with a view toward diagnosis and intervention.
One of us, Kristin Myers, studies the biology of tissue remodeling to quantify the biomechanics of pregnancy. Her lab creates computer models to measure how the uterus, cervix and fetal membranes work to carry the mechanical loads that pregnancy generates. She and her team use ultrasound to look at how the uterus grows and stretches and how much mechanical load is on the cervix, predicting whether it will fail too soon. Using the uterus as a pressure gauge for the mechanical environment of pregnancy could help identify problems before they occur.
Another of us, Michelle Oyen, studies the physics and materials science of soft tissues focusing on the mechanical properties of the fetal membranes and nutrient transport in the placenta. Her lab, along with Myers’ team, is applying big data and machine learning to anonymized medical records to create digital twins – or computational models of a given patient’s health data – that could help predict how a pregnancy will unfold. This may help physicians treat or avoid pregnancy complications.
Finally, Melissa Skala uses a noninvasive technique called optical coherence tomography. This imaging method produces 3D images of tissues that can’t be captured by ultrasound or MRI, such as extremely thin fetal membranes. Her lab used this technique to study how fetal membranes rupture under different pressures, providing a baseline of information that can be used to build better digital models of fetal membrane stress. Improved imaging of the fetal membranes and cervix can alert physicians to when these structures are at risk of failing.
Better imaging and better models
The Holy Grail of preterm birth prevention is early diagnosis. An early warning checklist for preterm birth risk could help protect the health of both baby and mother.
This checklist could look like your doctor ordering an imaging scan as soon as you find out you’re pregnant to understand the size of your uterus and cervix. Then they might take a swab of vaginal fluid to analyze biological changes in your cervix.
Better modeling techniques would be able to assess how your pregnancy will progress, and more precise imaging tools could measure changes over time. With a better prediction for when labor will start, doctors and patients can make a more informed decision on whether a C-section is necessary.

An accurate early warning checklist for preterm birth is still years away. But researchers in reproductive biology, epidemiology, bioinformatics and engineering are working hard to better understand in greater detail how babies are born and the many complications that can arise along the way, including preterm birth.
We believe that engineering – creative problem-solving using technology – is a critical addition to the multidisciplinary approach needed to address the complexity of preterm birth.
Melissa Skala receives funding from the National Institutes of Health and the National Science Foundation.
Kristin Myers receives funding from the National Institutes of Health, the National Science Foundation, and The Iris Fund.
Michelle L. Oyen receives funding from Wellcome Leap as part of the In Utero program, and from the National Institutes of Health. Michelle is an Associate Fellow of Homerton College, Cambridge.
This article was originally published on The Conversation. Read the original article.