Researchers have finally uncovered a multiorgan pathway with important implications for the pathogenesis of Long COVID. Several hypotheses have been proposed to explain the causes of Long COVID. These include the presence of a viral reservoir long after initial infection; chronic inflammation, development of antibodies (as a result of anti-viral responses) that mistakenly target and damage a person’s own tissues or organs; platelet dysfunction and increased tendency to form blood clots inside blood vessels; and finally autonomic nervous system dysfunction in which the nervous system cannot control processes like heart rate or blood pressure. In addition, people suffering from Long COVID also exhibit reduced levels of peripheral serotonin, which prevents the activity of the vagus nerve system, which transmits signals between the body and the brain, thus impairing hippocampal responses and memory.
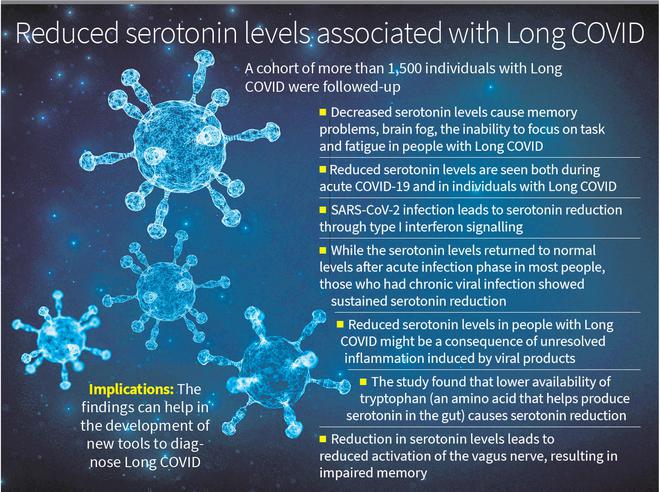
A study published recently in the journal Cell, researchers from the University of Pennsylvania, Philadelphia, who led the study, have found reduced levels of serotonin, a neurotransmitter, being associated with Long COVID. Memory problems, brain fog, and the inability to focus on tasks that people with Long COVID seem to suffer from might be due to reduced serotonin, the authors say. They followed a cohort of more than 1,500 individuals with Long COVID and characterised their spectrum of symptoms.
Dr. Maayan Levy from the University of Pennsylvania and one of the corresponding authors of the paper tweeted that serotonin levels are “reduced both during acute COVID-19 and in individuals with multiple long-term symptoms”, and the “phenomenon of serotonin reduction was not unique to SARS-CoV-2 infection since we also observed it in humans and mice acutely or chronically infected with other viruses,” she added.
The researchers went a step further by conducting animal studies by infecting mice expressing human ACE2 receptors with the ancestral strain of SARS-CoV-2. As expected, the mice infected exhibited reduced circulating serotonin. The same phenomenon was observed when wildtype mice were infected with the beta variant of SARS-CoV-2 and vesicular stomatitis virus (VSV).
The researchers found that SARS-CoV-2 infection led to serotonin reduction through type I interferon signalling; there is sustained elevation of interferons in people with Long COVID. According to Dr. Levy interferons reduce the serotonin level though three mechanisms — “reduced intestinal uptake of tryptophan, the biosynthetic precursor of serotonin; reduced counts of platelets, which carry serotonin in the circulation; and enhanced enzymatic turnover of serotonin”.
While in most people the serotonin levels returned to normal levels after the acute infection phase, those who had chronic viral infection showed sustained serotonin reduction. “We thus speculated that reduced serotonin levels in people with Long COVID might be a consequence of unresolved inflammation induced by viral products,” they write. They tested their hypothesis by recreating viral-induced inflammation in mice using synthetic RNA. This led to sufficient reduction in serotonin levels in total plasma and in isolated platelets. Normal serotonin levels were restored within a week of stopping synthetic RNA administration.
The researchers next investigated the mechanisms by which viral-induced inflammation reduced serotonin levels. Since the plasma tryptophan (an amino acid that helps produce serotonin in the gut and carries messages between nerve cells in the brain and throughout the body) levels are reduced in people during the acute COVID-19, in people with Long COVID and also in mice that were administered synthetic RNA repeatedly, they investigated whether serotonin production during viral infection was limited by reduced tryptophan availability. The mice study suggested that “lower tryptophan availability may cause serotonin reduction”. This was demonstrated when mice fed a tryptophan-deficient diet showed reduced plasma serotonin levels. Tryptophan uptake was also abrogated in mice treated with synthetic RNA.
The study also found that viral persistence in the gastrointestinal tract was associated with the development of Long COVID. While viral RNA was detectable in stool samples of a subset of individuals with Long COVID, those who did not have Long COVID did not show viral RNA in stool samples.
They found viral inflammation impaired serotonin storage. Circulating serotonin is transported into platelets. Platelet counts strongly decrease after acute VSV infection and synthetic RNA injection provide a possible explanation for reduced circulating serotonin levels. Other studies carried out by the team demonstrated that viral inflammation led to platelet hyperactivation, resulting in increased tendency to form blood clots and platelet count in the blood reaching very low levels in an interferon-dependent manner. As a result, platelet-mediated systemic serotonin transport is impaired.
They found serotonin turnover was enhanced during viral inflammation as revealed by increased serotonin degradation product in the urine of virally infected mice and in mice injected with synthetic RNA.
The researchers found that a reduction in serotonin levels leads to “reduced activation of the vagus nerve, resulting in neurocognitive manifestations, such as impaired memory. Interventions that restored serotonin levels or vagal activity prevented memory impairment”.
“We hope that our discovery will inspire clinical studies that use these insights to develop new tools for the diagnosis, monitoring, and treatment of Long COVID. They are so urgently needed,” Dr. Levy tweeted.







