Experts have made it clear that the end of the COVID-19 national emergency, which was lifted on May 11, 2023, does not mean an end to the pandemic. But this shift signals a remarkable turning point in a pandemic that is well into its fourth year – something that few could have imagined when the U.S. national emergency went into effect in March 2020.
Likewise, the World Health Organization’s announcement on May 5 that it was ending the COVID-19 public health emergency of international concern that had been in place since January 2020 is indicative that the pandemic has entered a new chapter.
It’s daunting to look back at our coverage and narrow it down to just a handful of standout stories amid all the twists and turns of the pandemic. But here are five stories from The Conversation’s archives that resonated with us, written by scholars who helped to illuminate complex issues at pivotal moments in the pandemic.
1. A whole new vocabulary
It’s a little hard to remember the days when words like pandemic, endemic diseases, mRNA, variant and spike proteins were not a part of our vernacular or everyday conversations. But I vividly recall the day that the COVID-19 pandemic was declared and a friend asked me “What exactly is a pandemic?” It turns out a lot of people were asking that question and wondering about the difference between an outbreak of an infectious disease, an epidemic and a pandemic.
Rebecca S.B. Fischer, an assistant professor of epidemiology at Texas A&M University, put it in straightforward terms: An outbreak is a small but unusual increase in the expected number of cases of a given disease, while the term epidemic is used when an infectious disease outbreak is getting bigger and spreading over a broader geographic area. A pandemic, on the other hand, is used when a disease is “international and out of control.”
She went on to say that some epidemiologists reserve the term pandemic for when a disease is being sustained in newly affected regions through local transmission – a good characterization of the state of COVID-19 in March 2020.
Read more: What's the difference between pandemic, epidemic and outbreak?
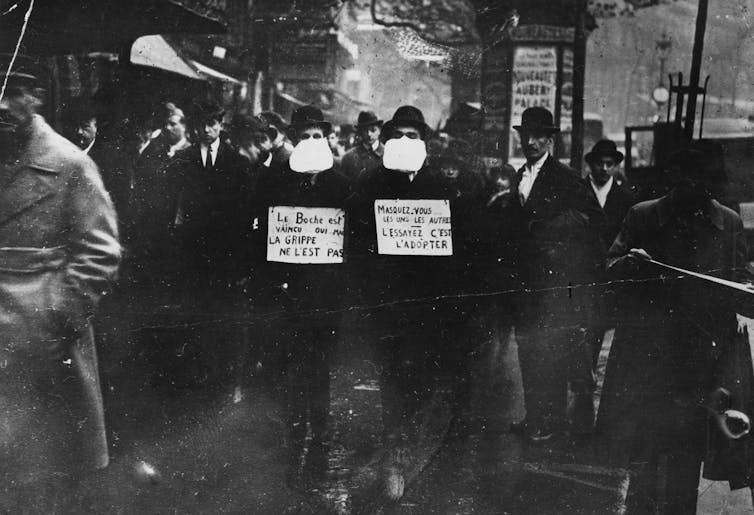
2. Comparisons to the 1918 flu ran rife
From the earliest days of the COVID-19 pandemic, it was impossible to miss the haunting similarities between it and the 1918 flu pandemic, which led to at least 50 million deaths worldwide between 1918 and 1920. Health care experts and the media made frequent comparisons between the two, pointing to similarities in attitudes about mask-wearing and school closures as well as in the patterns of disease waves, spikes and surges.
But while the two once-in-a-century events have shared plenty of likenesses, the comparison also sometimes led to public misunderstandings about how the COVID-19 pandemic could play out, wrote historian Mari Webel and pediatric infectious disease specialist Megan Culler Freeman, both from the University of Pittsburgh. They explain that key differences in the sociopolitical context of the 1918 flu period, as well as marked differences between the virology behind the two diseases, set the 1918 flu and COVID-19 on different paths.
“People seek answers from the experiences of influenza in 1918-19 for a fundamental reason: It ended.”
Read more: Compare the flu pandemic of 1918 and COVID-19 with caution – the past is not a prediction
3. How and when pandemics end
In late 2020, people were naturally wondering when and how the COVID-19 pandemic would end, and how we would know it was over.
Nükhet Varlik, a historian from Rutgers University who studies disease, medicine and public health, wrote an astute piece in October 2020 about the difficulties of predicting how the pandemic might play out. She presciently noted that “whether bacterial, viral or parasitic, virtually every disease pathogen that has affected people over the last several thousand years is still with us, because it is nearly impossible to fully eradicate them.” These include diseases like tuberculosis, leprosy, measles and plague.
“Hopefully COVID-19 will not persist for millennia,” Varlik wrote. But she went on to say that politics are crucial, noting how when vaccination programs are weakened, infections can “come roaring back.”
“Given such historical and contemporary precedents, humanity can only hope that the coronavirus that causes COVID-19 will prove to be a tractable and eradicable pathogen. But the history of pandemics teaches us to expect otherwise.”
Read more: How do pandemics end? History suggests diseases fade but are almost never truly gone
4. The midway point
The summer of 2021 felt like a particularly grueling moment in time – when excitement and optimism over the launch of the first vaccines to protect against COVID-19 had given way to despair over the stronghold of vaccine resistance and general exhaustion with all things COVID. And then came the delta variant.
Epidemiologist Katelyn Jetelina from the University of Texas Health Science Center at Houston captured 18 months of the COVID-19 pandemic in a series of seven retrospective charts that put all of the high and low points into stark relief. “The race between vaccination and variant spread was upon us,” Jetelina wrote. “The fight was far from over.”
The same may still be true today.
Read more: 18 months of the COVID-19 pandemic – a retrospective in 7 charts
5. How omicron altered the course of the pandemic
When the omicron variant arrived on the scene in late 2021 and spread globally in early 2022, it soon became clear that it could bring about a shift in the pandemic. With its ability to spread easily and to also cause milder disease than prior variants, omicron had the potential to act as a natural vaccine of sorts – producing widespread immunity with the help of the existing COVID-19 vaccines.
But the omicron variant had plenty of surprises in store. For one, it gave rise to a family of variants and sublineages that to this day are keeping researchers guessing, with the latest omicron subvariant, XBB.1.16, gaining ground across the U.S. and worldwide as of mid-May 2023.
In January 2022, immunology researchers Prakash Nagarkatti and Mitzi Nagarkatti, from the University of South Carolina, explained how the immune system responds to infections and how it remembers those threats through “immunological memory.”
This left room for hope, they wrote, that “when new variants of SARS-CoV-2 inevitably arise, omicron will have left the population better equipped to fight them. So the COVID-19 vaccines combined with the omicron variant could feasibly move the world to a new stage in the pandemic – one where the virus doesn’t dominate our lives and where hospitalization and death are far less common.”
Read more: Is the omicron variant Mother Nature’s way of vaccinating the masses and curbing the pandemic?
Editor’s note: This story is a roundup of articles from The Conversation’s archives.
This article was originally published on The Conversation. Read the original article.







