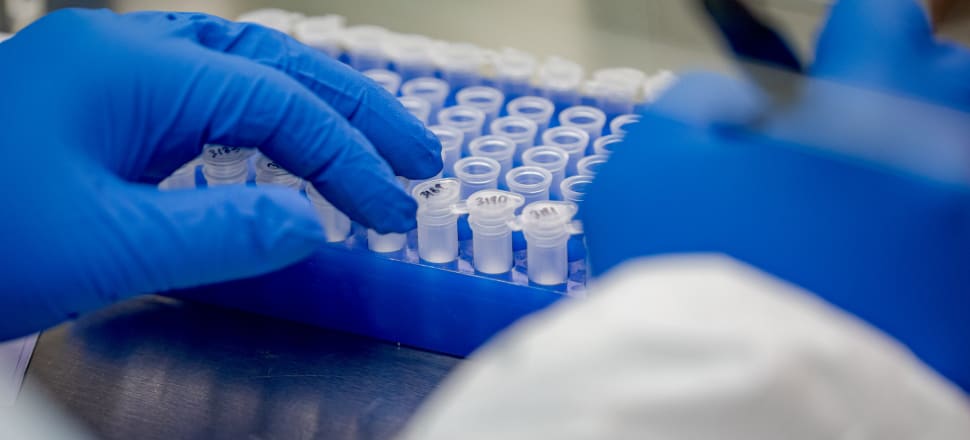
Kiwi labs looked anxiously at Omicron outbreaks overseas and warned officials about the impending pressure on testing – only to seemingly be ignored. Now, they say structural change is needed to avoid a repeat, Sam Sachdeva reports.
New Zealand’s laboratory network has come under the microscope in the wake of a review into a Covid testing collapse, with the sector calling for greater investment in staff and a larger role in national planning.
An independent report on why the country’s PCR testing systems were overwhelmed during the Omicron outbreak earlier this year found the backlog was predictable and could have been avoided.
Among the deficiencies raised by the review was the “confusion, mixed messaging and delay in communication” between the ministry, DHBs and the labs due to a lack of clear governance arrangements and multiple lines of communication.
Throughout the pandemic, labs had worked with the ministry under a “letter of agreement” which set out a fixed price per test, but did not include any expectations around capacity or means of managing Covid testing from a national perspective.
“Unable to enforce compliance, the ministry’s relationship with the network has therefore been reactive and relied on good will to influence capacity planning.”
With a lack of signals from the ministry in relation to the ‘standing capacity’ labs were expected to have, there had been no incentive for them to develop capacity other than in a reactive way.
“It was clear to the laboratories that once in the community, Omicron would spread quickly, and testing demand would spike. It was also apparent that positivity rates would increase rapidly, and sample pooling would be impacted quickly." – independent review
After labs were pushed by the extraordinary demands of the Delta outbreak, in late 2021 they were speaking with the ministry’s testing group about their experience in the hopes it would help in a future outbreak.
Among their key messages were that “PCR testing capacity was finite and meeting outbreak demand through PCR testing was dependent on sample pooling [which was] not sustainable and becomes increasingly less efficient as positivity rates increase”.
Labs also claimed to have advised the ministry about the impact on pooling if Covid positivity rates were at three, five and 10 percent, and had kept in close contact with their Australian colleagues about the country’s experience as its PCR testing became overwhelmed.
“It was clear to the laboratories that once in the community, Omicron would spread quickly, and testing demand would spike. It was also apparent that positivity rates would increase rapidly, and sample pooling would be impacted quickly."
Since the transition to rapid antigen tests, the number of PCR tests being processed had fallen dramatically, and there was growing concern within the lab network about idle equipment and staff.
“Without a direction from the ministry on the future capacity requirements for PCR testing, there is a risk that laboratories will begin to dismantle their capacity, including mothballing equipment and reducing staffing.”
Systemic problems
Terry Taylor, the president of the New Zealand Institute of Medical Laboratory Science, told Newsroom the review highlighted the "systemic" problems within New Zealand’s laboratory network as well as Covid shortcomings.
“When you look at this whole situation, for me, it personally goes back about 15 years when they started contracting out our services.”
Taylor said the lab system was largely run by the providers, not district health boards or the ministry, which meant officials had limited control to address some of the flaws which emerged.
While the review had highlighted the small size of the ministry’s laboratory testing team, there was also too much bureaucracy surrounding them and no direct line to leadership.
Taylor said he and others had spoken out about Australia’s own testing woes in January both to raise the alert and ensure that lab staff did not get blamed if there was a similar outcome here.
“I've got no two ways that if we didn't as a professional body stand up and say, ‘Look, these are the warning signs, this is what's going to happen, our workforce is a limited resource, and you're not using them the way they should be’…it's the laboratory staff on the ground getting blamed for that and that wouldn't have been fair at all.”
There needed to be greater collaboration between labs and the ministry, and greater investment into and support for the workforce, he said.
Speaking to media about the review’s findings earlier this week, Director-General of Health Dr Ashley Bloomfield said ministry officials had been meeting with lab representatives “on an almost daily basis” and enjoyed a strong relationship.
Long-standing issues around the delivery of lab services in the country had become increasingly stark as the Omicron outbreak placed strain on the system, Bloomfield said.
Green Party Covid response spokesman Teanau Tuiono told Newsroom the review’s findings were “a strong signal that our public health system needs to be properly public” and not privately run.
One particular problem was the different IT systems of labs around the country, which made it near-impossible to move samples from overloaded regions to other areas.
New contracts being drawn up for the ministry’s relationship with the labs would include a requirement for interoperability with a national database, as well as conditions around PCR capacity to ensure testing could ramp up if needed in future.
Asked by Newsroom whether the health system’s reliance on private labs for a significant proportion of medical testing was still set for purpose, Bloomfield said that was a longer-term debate which would cover other areas like radiology and surgical services.
“If we look at the role that our labs have played and that testing has played in New Zealand's response to the outbreak, it's been fundamentally successful, our ability to ramp up PCR testing capacity across both public and private, their willingness to work together and certainly their willingness to engage in the discussion about this next phase as well.”
Bloomfield emphasised the testing delays that occurred were not the fault of the country’s lab staff, who had processed over seven million Covid tests since the onset of the pandemic in March 2020.
While he did not know why some lab workers were leaving the profession, it was important the workforce was adequately paid and looked after.
Green Party Covid response spokesman Teanau Tuiono told Newsroom the review’s findings were “a strong signal that our public health system needs to be properly public” and not privately run.
"It's clear we need to invest in allied healthcare, including pay equity, and long-term investment in the pandemic workforce because Covid-19 is still here, and it won't be the last pandemic we face," Tuiono said.